Volume 6, Issue 3 (2025)
J Clinic Care Skill 2025, 6(3): 137-145 |
Back to browse issues page
Article Type:
Subject:
Ethics code: IR.FUMS.REC.1400.153),
History
Received: 2025/05/10 | Accepted: 2025/06/23 | Published: 2025/07/2
Received: 2025/05/10 | Accepted: 2025/06/23 | Published: 2025/07/2
How to cite this article
Kouhi F, Bijani M, Fereidouni Z, Dehghan A, Taghinezhad A. Effect of the Orem-Based Self-Care Education Model on Improving the Quality of Life and Health-Promoting Lifestyle in Hypertensive Patients. J Clinic Care Skill 2025; 6 (3) :137-145
URL: http://jccs.yums.ac.ir/article-1-431-en.html
URL: http://jccs.yums.ac.ir/article-1-431-en.html
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



Rights and permissions
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
1- Student Research Committee, Fasa University of Medical Sciences, Fasa, Iran
2- Department of Medical-Surgical Nursing, Faculty of Nursing, Fasa University of Medical Sciences, Fasa, Iran
3- Noncommunicable Diseases Research Center (NCDRC), Fasa University of Medical Sciences, Fasa, Iran
4- Department of Foreign Languages, Faculty of Medicine, Fasa University of Medical Sciences, Fasa, Iran
2- Department of Medical-Surgical Nursing, Faculty of Nursing, Fasa University of Medical Sciences, Fasa, Iran
3- Noncommunicable Diseases Research Center (NCDRC), Fasa University of Medical Sciences, Fasa, Iran
4- Department of Foreign Languages, Faculty of Medicine, Fasa University of Medical Sciences, Fasa, Iran
Full-Text (HTML) (245 Views)
Introduction
Hypertension (HTN) is the major modifiable risk factor for heart disease, stroke, and kidney failure, and it is the leading cause of death as well as the second leading cause of lost disability-adjusted life-years worldwide [1]. Globally, the prevalence and total burden of HTN are increasing, particularly in countries with low and middle incomes [2]. It is predicted that around 29.0% of women and 26.0% of men will have HTN by 2025 [3]. The global burden of HTN is projected to exceed 1.6 billion by 2025 [4]. The escalating prevalence of HTN constitutes a critical threat to global public health, with current estimates attributing approximately 17 million deaths annually to this condition. In Iran, national statistics indicate that nearly 46% of the population is affected by HTN, underscoring its considerable burden on the healthcare system and the population at large [5, 6]. As a leading contributor to approximately 45% of cardiovascular-related deaths and more than half of all cerebrovascular fatalities, HTN continues to exert profound clinical consequences. These outcomes are largely attributable to its asymptomatic presentation and insidious progression, characteristics that have earned it the designation of “silent killer” [7, 8].
The World Health Organization defines quality of life (QoL) as an individual’s perception of their position in life, situated within the context of their cultural values, belief systems, personal goals, physical health, psychological state, social relationships, and environmental circumstances [9, 10]. In the context of nursing practice, promoting QoL is not merely an aspirational goal but a fundamental component of patient-centered care. Achieving this outcome necessitates a multifaceted approach that extends beyond pharmacological treatment and emphasizes active patient involvement in self-care and long-term disease management [11].
Self-care education equips individuals with the necessary knowledge and practical skills to take responsibility for their own health, thereby fostering autonomy, preserving functional capacity, and slowing the progression of chronic diseases [12]. Among the various theoretical frameworks guiding such interventions, Orem’s self-care theory remains one of the most comprehensive and contextually adaptable models. This framework provides a systematic approach to identifying self-care deficits, assessing patient needs, and delivering tailored support, particularly for individuals managing long-term conditions such as HTN [13].
Orem’s self-care model has been designed to promote care based on the conditions and needs of individuals experiencing a deviation from normal health and emphasizes the role of caregiving through a wholly compensatory system, a partly compensatory system, and a supportive-educative system. In the wholly compensatory system, the nurse is responsible for the patient’s entire care plan to compensate for the patient’s inability to perform self-care. In the partly compensatory system, both the nurse and the patient participate in self-care. The supportive-educative system is implemented when the patient is ready to learn to perform an activity but is unable to do so without support and education—in this situation, the nurse primarily acts as an educator and advisor [14, 15]. In the present study, the researchers utilized the supportive-educative system defined by Orem’s self-care model.
Given the high prevalence of HTN and its well-established association with life-threatening complications, including myocardial infarction and cerebrovascular accidents, the development and implementation of evidence-based, patient-centered educational strategies are of paramount importance. Most studies in this field have been conducted descriptively, and the few available experimental studies have not utilized Orem’s self-care model. Although previous studies have demonstrated the impact of educational interventions using various models, including Pender’s health promotion model and the health belief model, to enhance the QoL and self-care behaviors of hypertensive patients [16, 17], few studies have investigated the effect of an educational program using Orem’s self-care model in hypertensive patients. Thus, due to the significance of the subject and the limited research conducted in this area, it is recommended that the present study be carried out in different countries to facilitate knowledge translation in patient education. Accordingly, the present study was designed to determine the impact of an educational program using Orem’s self-care model on improving the QoL and health-promoting lifestyle in hypertensive patients in the south of Iran.
Materials and Methods
Study design and sample
This prospective, open-label randomized controlled trial was implemented at two tertiary cardiovascular referral centers located in southern Iran and spanned an eight-month period, from August 2022 to April 2023. Due to the inherently interactive nature of the intervention, blinding of participants and providers was not feasible and therefore was not employed.
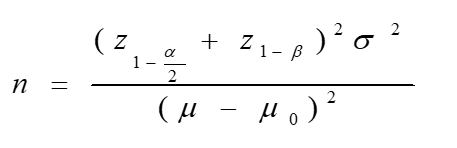
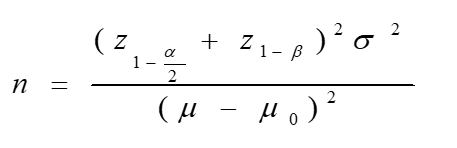
The sample size was calculated based on statistical parameters reported by Jamshidi et al. [12], utilizing assumptions appropriate for comparing mean values across two related groups. Assuming a two-tailed significance level (α) of 0.05 and a statistical power (1-β) of 90%, the minimum required sample size for each group was determined to be 28 participants. To account for potential attrition and to enhance the statistical power of the analysis, the sample size was deliberately increased, resulting in the allocation of 40 participants to each group. This adjustment was made to strengthen analytical robustness and improve the generalizability of the study findings.
Inclusion and exclusion criteria were precisely defined to ensure methodological rigor in participant selection. Eligible participants were adults aged between 30 and 55 years with a confirmed clinical diagnosis of HTN who provided written informed consent. Individuals were excluded if they experienced acute clinical deterioration during the study period or voluntarily withdrew their participation at any stage. Such exclusions were applied to preserve the internal validity of the study and to ensure the integrity of the final analysis.
From an initial cohort of 94 individuals diagnosed with HTN, participants were recruited using a non-random convenience sampling method. Following an eligibility assessment based on predefined inclusion criteria, 14 individuals were excluded due to non-compliance with the study’s entry requirements. The final sample comprised 80 participants, who were then randomly assigned to two equal groups: the experimental arm (n=40) and the control arm (n=40).
Random allocation was carried out through a straightforward yet rigorously controlled concealment procedure. Eighty identical cards, with half labeled “A” and the other half labeled “B,” were thoroughly shuffled and placed in a sealed, opaque container to mitigate selection bias. Each eligible participant was instructed to draw a card blindly. Those who selected “A” were assigned to the intervention group, while those who drew “B” were allocated to the control group. A detailed account of participant recruitment, allocation, retention, and follow-up is visually presented in the CONSORT flowchart (Figure 1).
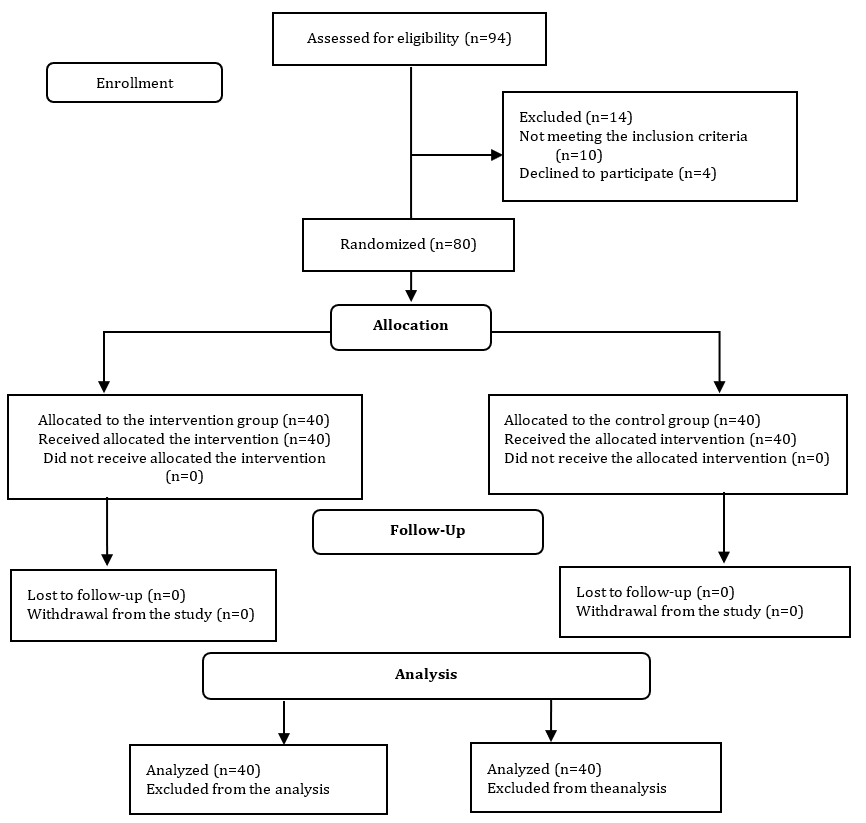
Figure 1. CONSORT flow diagram of the participants throughout the study
Study procedure
Prior to the commencement of the study, full ethical approval was obtained from the Institutional Review Board (IRB) of the affiliated academic institution. Following protocol approval, a formal authorization letter was issued by the Office of the Vice-Chancellor for Research. Upon arrival at the clinical site, the principal investigator provided prospective participants with a clear and comprehensive explanation of the study’s objectives, scope, and procedures. Both verbal and written informed consent were obtained from individuals who agreed to participate.
The educational intervention, meticulously designed in alignment with Dorothea Orem’s self-care theoretical framework, consisted of six structured instructional sessions, each lasting approximately two hours. To preserve group integrity and prevent cross-contamination, sessions were conducted separately for the two groups. Each session accommodated approximately 20 participants, ensuring an optimal facilitator-to-participant ratio conducive to meaningful interaction. The instructional approach incorporated didactic lectures, interactive discussions, and the distribution of printed educational materials. In response to the ongoing COVID-19 pandemic, all sessions strictly adhered to public health guidelines, including physical distancing and routine sanitization.
The educational content was closely aligned with the central tenets of Orem’s model and tailored to address the complex self-care needs of adults managing HTN. Curriculum topics included the physiological mechanisms underlying blood pressure regulation, etiological factors contributing to HTN, and the systemic consequences of uncontrolled blood pressure. Instruction emphasized the development of self-management competencies across several key domains: initiation of regular physical activity, adherence to dietary recommendations, weight management, stress regulation, and engagement in mind-body practices such as diaphragmatic breathing, yoga, and meditation. Additional content focused on risk-reduction behaviors, including smoking cessation, abstinence from alcohol, adherence to prescribed pharmacologic treatments, accurate self-monitoring of blood pressure, and maintenance of routine medical follow-ups.
Each of the six sessions addressed a distinct thematic focus. Session 1 provided an overview of blood pressure physiology, definitions of HTN, and associated health risks; Session 2 explored modifiable and non-modifiable risk factors, along with the long-term complications of poorly controlled HTN; Session 3 introduced the concept of self-care and outlined empirically supported strategies for chronic disease management; Session 4 focused on behavioral lifestyle modifications, including exercise planning, nutritional practices, body weight regulation, and stress coping techniques; Session 5 examined integrative therapies, such as controlled breathing, yoga, and meditation, and addressed the health risks linked to tobacco and alcohol use; and Session 6 featured a hands-on demonstration of home blood pressure monitoring techniques and reinforced the importance of ongoing clinical engagement and medication adherence.
Participants in the intervention group attended all six sessions and had continuous access to expert facilitators who addressed individual questions to ensure thorough comprehension of the material. Printed pamphlets were also provided as supplementary educational resources. In contrast, the control group did not receive any instructional content during the intervention period. However, in accordance with ethical considerations, control participants were given the same informational pamphlets upon completion of the study.
Data collection was conducted at four distinct time points; prior to the intervention (baseline), immediately after the final session, one month following the intervention, and again at the three-month follow-up. At each interval, participants completed validated self-report instruments under the direct supervision of trained research personnel, and blood pressure measurements were performed using standardized clinical procedures.
Prior to participation, all individuals were comprehensively informed about the study’s objectives, methodological procedures, and data usage protocols. Written informed consent was subsequently obtained. Participant confidentiality and anonymity were rigorously preserved throughout the data collection, management, and analysis phases. All procedures adhered strictly to institutional ethical guidelines and the principles outlined in the Declaration of Helsinki. In cases involving legally dependent individuals, informed consent was additionally obtained from authorized legal guardians or representatives.
Instrument
A comprehensive battery of empirically validated tools was employed to facilitate multidimensional data collection. These included a demographic data form, the Short Form-36 Health Survey (SF-36), the Health-Promoting Lifestyle Profile (HPLP), and the Hypertension Self-Care Profile (HTN-SCP), each selected for its established psychometric reliability and direct relevance to the study objectives.
The demographic questionnaire comprised 13 systematically constructed items designed to capture essential sociodemographic and clinical parameters. Collected data included chronological age, gender identity, educational attainment, occupational status, marital status, smoking behavior, systolic and diastolic blood pressure readings, body mass index (BMI), presence of comorbidities, duration since HTN diagnosis, and history of medical consultations related to hypertensive care.
To assess participants’ perceived health-related QoL, the study employed the SF-36, originally developed by Ware & Sherbourne [18]. The Persian-language version, previously translated and psychometrically validated by Montazeri et al. [19], was utilized. This 36-item instrument encompasses eight multidimensional domains, including physical functioning, role limitations due to physical health, role limitations due to emotional problems, vitality, mental health, social functioning, bodily pain, and general health perceptions. Each domain is scored on a scale from 0 to 100, with higher scores reflecting better perceived health status and overall QoL.
Lifestyle behaviors associated with sustained health promotion were evaluated using the Health-Promoting Lifestyle Profile (HPLP), originally developed by Walker & Hill-Polerecky [20]. This instrument measures six critical dimensions of health behavior, including nutrition, physical activity, health responsibility, interpersonal relations, stress management, and self-actualization. Its Persian version, psychometrically validated by Mohammadi Zeidi et al. [21], comprises 52 items rated on a four-point Likert scale ranging from 1 (never) to 4 (routinely). Cumulative scores indicate the extent to which individuals engage in behaviors conducive to health promotion.
HTN-specific self-care competencies were assessed using the Hypertension Self-Care Profile (HTN-SCP), developed by Han et al. [22]. Although initially validated among Korean American populations, the instrument was later culturally adapted and validated for use among Iranian adults by Mohammadnejad et al. [23]. The HTN-SCP consists of 20 items spanning four principal domains: adherence to dietary and exercise recommendations, compliance with prescribed medications, ability to interpret nutritional labels, and general self-management of HTN. Each item employs a four-point response scale, with higher scores indicating greater adherence to recommended self-care behaviors.
Statistical analysis
Data analyses were conducted using SPSS 22. Between-group differences were assessed using independent sample t-tests for continuous parameters and Chi-square tests for categorical parameters. To examine within-group changes over time, repeated measures analysis of variance (ANOVA) was employed, allowing for the longitudinal evaluation of intervention effects across multiple time points.
Findings
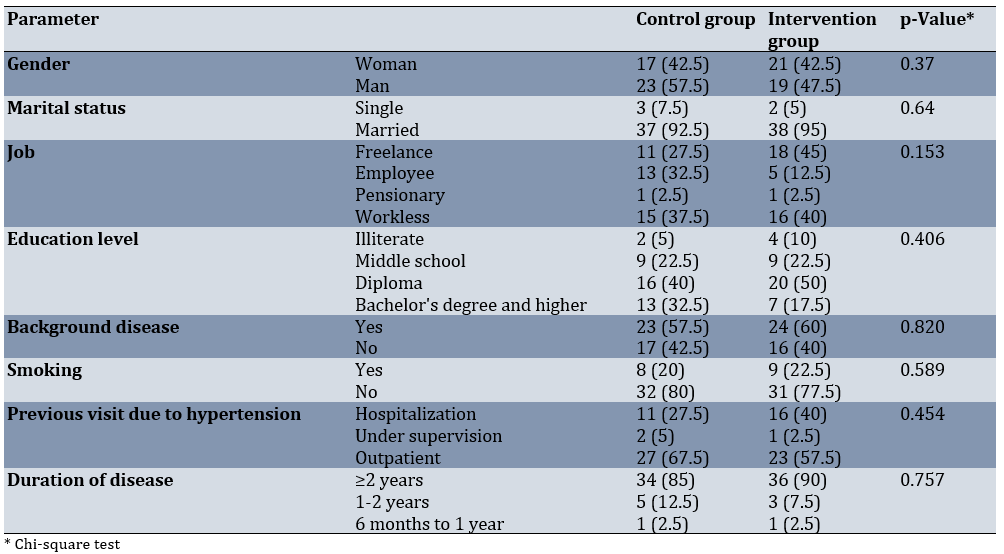
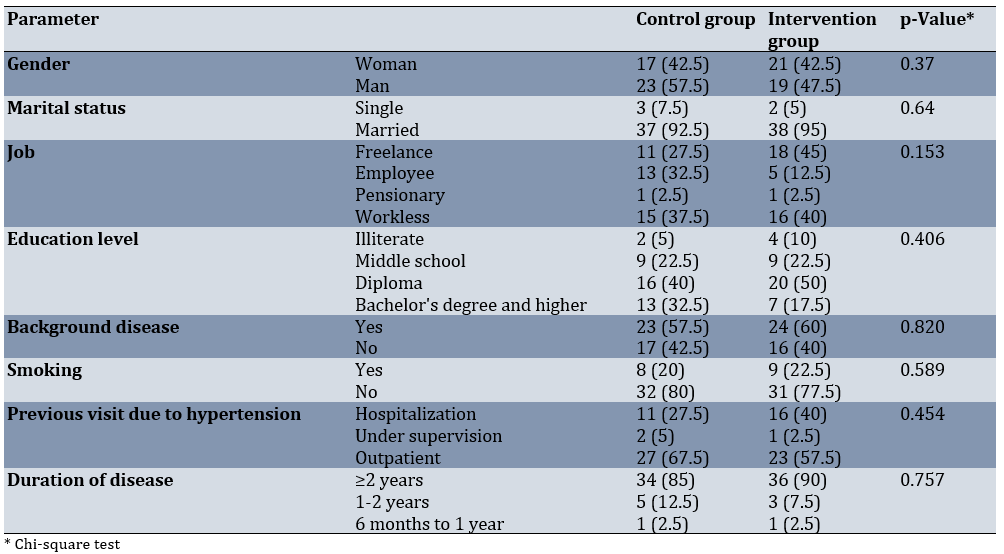
The final analytical sample comprised 80 adult participants with a confirmed diagnosis of HTN, with a mean age of 44.16±4.60 years. The mean age in the control and intervention groups was 44.80±5.09 and 43.53±4.13 years, respectively (p=0.222). Baseline demographic characteristics showed no statistically significant differences between the experimental and control groups, thereby confirming the initial comparability of the cohorts. Similarly, pre-intervention QoL scores did not exhibit any meaningful intergroup differences (Table 1).
Table 1. Demographic information of the subjects
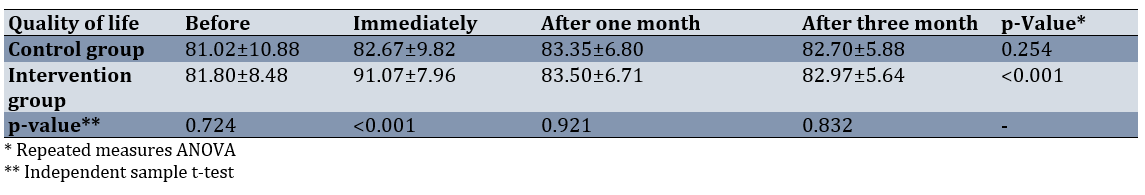
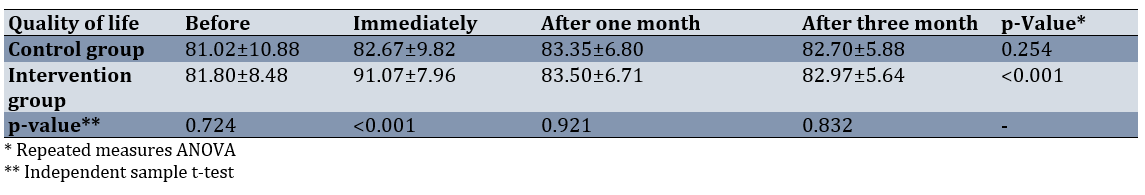
Post-intervention assessments, however, revealed statistically significant improvements in QoL among participants in the educational intervention group. These enhancements were sustained at both the one-month and three-month follow-up assessments compared to the control group (p<0.001; Table 2).
Table 2. Comparing the mean quality of life scores in the groups before and after the educational intervention
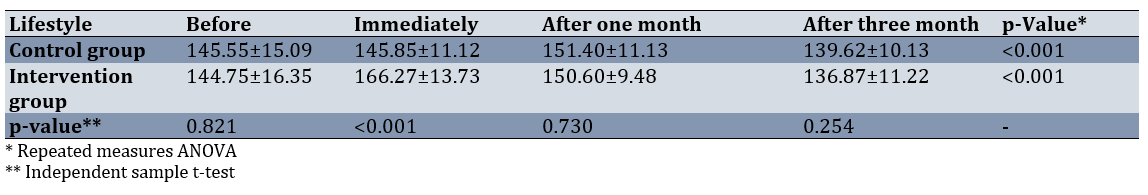
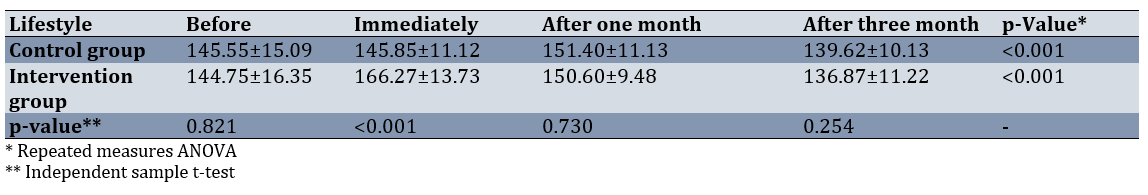
Although no significant differences in health-promoting lifestyle behaviors were observed at baseline, the intervention group demonstrated substantial and statistically significant improvements across all post-intervention time points (p<0.001; Table 3).
Table 3. Comparing the mean lifestyle scores in the groups before and after the intervention
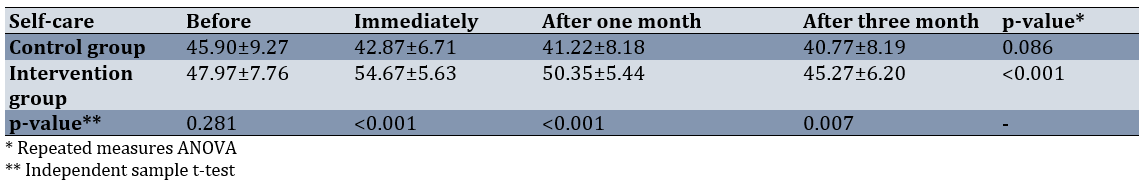
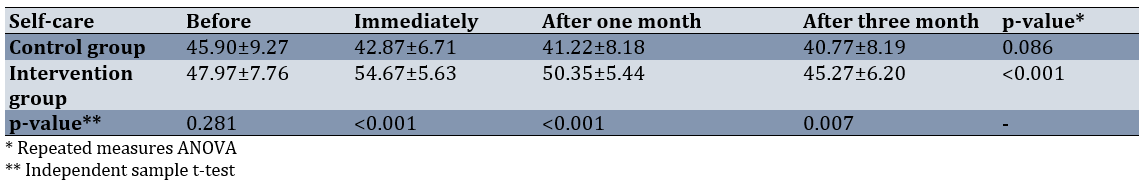
A similar pattern emerged in the domain of self-care efficacy. Baseline scores did not differ significantly between the two groups; however, participants in the intervention group exhibited marked improvements following the intervention. These gains remained statistically robust at both follow-up intervals (p<0.001; Table 4).
Table 4. Comparing the mean self-care scores in the groups before and after the intervention
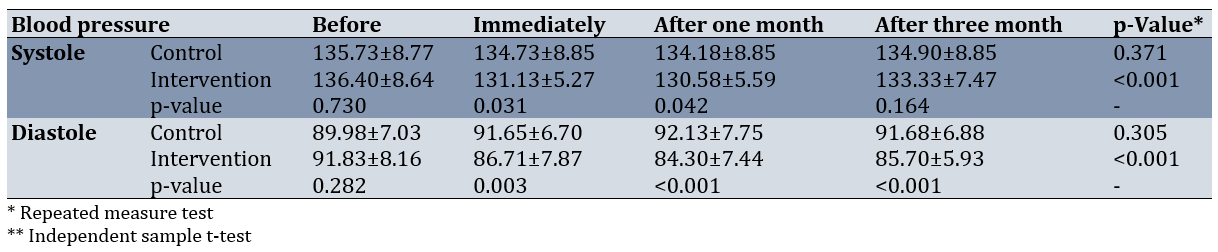
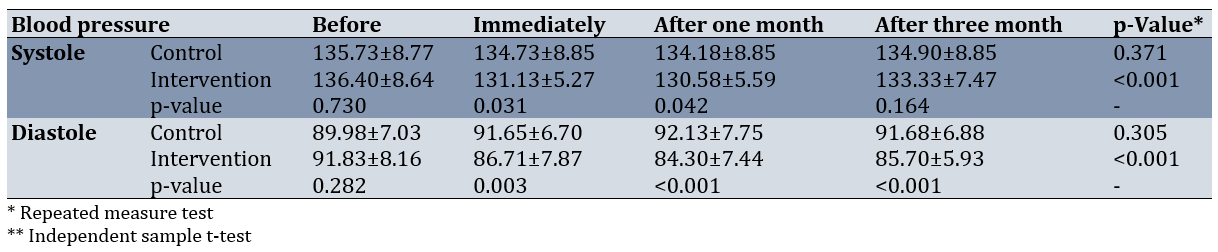
Regarding blood pressure outcomes, baseline systolic and diastolic values were statistically comparable between the groups. Notably, the intervention group experienced a significant reduction in systolic blood pressure immediately post-intervention and at the one-month follow-up. Although this reduction diminished slightly by the three-month evaluation, diastolic blood pressure levels in the intervention group continued to demonstrate statistically significant and clinically meaningful reductions across all follow-up time points (p<0.001; Table 5).
Table 5. Comparing the mean scores of systolic and diastolic blood pressures in the groups before and after the intervention
Discussion
This study systematically evaluated the effectiveness of a theory-driven self-care educational intervention, grounded in Orem’s conceptual model, in enhancing QoL and fostering health-promoting behaviors among individuals diagnosed with HTN. The equivalence of baseline characteristics across study arms served to strengthen the internal validity of the observed outcomes.
Following the implementation of the six-session instructional program, participants in the intervention group exhibited statistically significant improvements in both subjective well-being and self-regulatory health behaviors. While reductions in systolic blood pressure were apparent immediately post-intervention and at the one-month follow-up, this trend attenuated somewhat by the third month, suggesting a potential need for periodic reinforcement. In contrast, diastolic pressure reductions remained stable and statistically significant throughout the follow-up period, indicating a more durable physiological response to the intervention.
These findings are congruent with those of Bairami et al., reporting a strong association between active self-care engagement and improved QoL among individuals with chronic conditions. The current study extends this line of inquiry by providing additional empirical support for the efficacy of structured educational programs, particularly when underpinned by a well-established nursing theory. The results confirm that theoretically guided interventions can produce sustained improvements in both behavioral and clinical outcomes in hypertensive populations [24].
A substantial body of empirical research has underscored the critical role of lifestyle modification in optimizing clinical outcomes among individuals with chronic diseases. In a descriptive-comparative study, Zareei et al. demonstrate a clear and direct relationship between positive behavioral changes and enhanced health indices [25]. Consistent with this body of evidence, the present study documented significant improvements across multiple lifestyle dimensions following the implementation of a targeted self-care training program. Concurrent reductions in systolic and diastolic blood pressure provided further validation of the intervention’s effectiveness in mitigating cardiovascular risk.
Similar conclusions were drawn by Asa Kohneforoudi et al., who found that adherence to self-care practices significantly predicts higher levels of self-efficacy, a recognized psychosocial determinant of successful HTN prevention and management [26]. Their endorsement of individualized, behaviorally oriented interventions is reflected in the current study’s application of Orem’s theoretical framework, which informed the design of a personalized educational strategy. This model-based approach yielded measurable benefits in both cognitive-behavioral and physiological domains, thereby reinforcing its practical relevance and applicability in clinical settings.
Further empirical support for comprehensive self-management strategies was provided by Arabshahi et al., identifying a notable adherence gap, particularly regarding sodium restriction, despite relatively high compliance with medication use and physical activity guidelines. They reported that approximately 25% of patients are unable to effectively limit dietary sodium intake [27]. In alignment with these findings, the present intervention adopted a holistic perspective by integrating key components of HTN management, including nutritional modification, pharmacologic adherence, and physical activity promotion. This multidimensional approach contributed to significant and sustained reductions in both systolic and diastolic blood pressure, underscoring the necessity of comprehensive self-care education.
In a cross-national investigation conducted across three healthcare institutions in Sri Lanka, Pirasath et al. have identified widespread deficits in patient awareness concerning diagnostic criteria, treatment goals, and personal blood pressure targets, despite a general understanding of HTN risk factors. Although in the mentioned study, medication adherence is rated as satisfactory, memory lapses frequently is emerged as a principal barrier to consistent therapeutic compliance. In response, the authors have advocated for the implementation of individualized educational interventions [28]. Echoing this recommendation, the current study incorporated modular instruction covering key topics, such as the pathophysiology of HTN, potential complications, pharmacologic adherence, and the importance of regular medical follow-up. The observed improvements in patient-reported outcomes following the intervention provide compelling evidence for the efficacy of this educational model.
Ketata et al. report a constellation of risk factors associated with suboptimal self-care engagement, including advanced disease severity, the presence of comorbid respiratory conditions, limited formal education, and the absence of prior instruction in self-management strategies [29]. These findings highlight the importance of tailoring health education to reflect the sociodemographic and clinical profiles of target populations. Within this context, the present study’s implementation of a theory-informed, demographically sensitive intervention significantly enhanced participants’ self-care capabilities, thereby demonstrating its effectiveness in addressing diverse patient needs.
The critical importance of non-pharmacologic strategies in the management of HTN was reaffirmed by Carey et al., whose comprehensive guideline review positions lifestyle modification as the cornerstone of effective blood pressure control [30]. Their recommendations highlight several key behavioral targets, including dietary moderation (specifically, sodium reduction and potassium enrichment), balanced nutritional intake, routine physical activity, and responsible alcohol consumption. The empirical findings of the present study align closely with these best-practice recommendations. Participants in the intervention group demonstrated improved adherence to prescribed lifestyle modifications, which corresponded with statistically significant reductions in both systolic and diastolic blood pressure. These results suggest a synergistic relationship between enhancements in QoL and positive lifestyle behavioral changes, collectively contributing to sustained blood pressure regulation.
The participants were recruited from a single center in southern Iran, which may limit the generalizability of the findings. Another limitation of this study was the small sample size; it is recommended to use a larger population size in similar research. Additionally, the lack of blinding and the non-equivalent intervention intensity between groups, as well as the short time period between the intervention and the assessment of the patients’ outcomes, can be mentioned as limitations. It is further suggested that longitudinal and prospective cohort studies be conducted. Data were collected using self-reported measures such as self-efficacy and life satisfaction scores. Potential response bias may have resulted from participants providing answers they perceived as socially acceptable or that did not accurately represent their genuine emotions and experiences.
It is recommended that periodic booster sessions or continuous support mechanisms be instituted to maintain behavioral momentum, facilitate enduring lifestyle adjustments, and promote long-term hemodynamic stability.
Conclusion
The Orem-based self-care educational intervention leads to meaningful short-term improvements in QoL and health-promoting behaviors among individuals with HTN.
Acknowledgments: The authors express their sincere appreciation to the emergency medical personnel whose active participation and cooperation were instrumental to the successful execution of the study. The authors also extend special thanks to Fasa University of Medical Sciences for institutional support and to the Clinical Research Development Unit of Fasa Valiasr Hospital for their invaluable assistance with logistical coordination and financial oversight.
Ethical Permissions: The study protocol received ethical clearance from the Research Ethics Committee of Fasa University of Medical Sciences (Approval No. IR.FUMS.REC.1400.153), and all procedures adhered strictly to institutional ethical guidelines and the principles outlined in the Declaration of Helsinki. IRCT Registration Number: IRCT20190917044802N4.
Conflicts of Interests: The authors declared no conflicts of interests.
Authors' Contribution: Kouhi F (First Author), Methodologist/Assistant Researcher/Discussion Writer/Statistical Analyst (25%); Bijani M (Second Author), Introduction Writer/Methodologist/Main Assistant Researcher/Discussion Writer (35%); Fereidouni Zh (Third Author), Methodologist/Assistant Researcher/Statistical Analyst (30%); Dehghan A (Fourth Author), Introduction Writer/Methodologist/ Assistant Researcher (5%); Taghinezhad A (Fifth Author), Assistant Researcher/Discussion Writer/Statistical Analyst (5%)
Funding/Support: This research was conducted independently and did not receive funding from governmental agencies, commercial enterprises, or nonprofit organizations.
Hypertension (HTN) is the major modifiable risk factor for heart disease, stroke, and kidney failure, and it is the leading cause of death as well as the second leading cause of lost disability-adjusted life-years worldwide [1]. Globally, the prevalence and total burden of HTN are increasing, particularly in countries with low and middle incomes [2]. It is predicted that around 29.0% of women and 26.0% of men will have HTN by 2025 [3]. The global burden of HTN is projected to exceed 1.6 billion by 2025 [4]. The escalating prevalence of HTN constitutes a critical threat to global public health, with current estimates attributing approximately 17 million deaths annually to this condition. In Iran, national statistics indicate that nearly 46% of the population is affected by HTN, underscoring its considerable burden on the healthcare system and the population at large [5, 6]. As a leading contributor to approximately 45% of cardiovascular-related deaths and more than half of all cerebrovascular fatalities, HTN continues to exert profound clinical consequences. These outcomes are largely attributable to its asymptomatic presentation and insidious progression, characteristics that have earned it the designation of “silent killer” [7, 8].
The World Health Organization defines quality of life (QoL) as an individual’s perception of their position in life, situated within the context of their cultural values, belief systems, personal goals, physical health, psychological state, social relationships, and environmental circumstances [9, 10]. In the context of nursing practice, promoting QoL is not merely an aspirational goal but a fundamental component of patient-centered care. Achieving this outcome necessitates a multifaceted approach that extends beyond pharmacological treatment and emphasizes active patient involvement in self-care and long-term disease management [11].
Self-care education equips individuals with the necessary knowledge and practical skills to take responsibility for their own health, thereby fostering autonomy, preserving functional capacity, and slowing the progression of chronic diseases [12]. Among the various theoretical frameworks guiding such interventions, Orem’s self-care theory remains one of the most comprehensive and contextually adaptable models. This framework provides a systematic approach to identifying self-care deficits, assessing patient needs, and delivering tailored support, particularly for individuals managing long-term conditions such as HTN [13].
Orem’s self-care model has been designed to promote care based on the conditions and needs of individuals experiencing a deviation from normal health and emphasizes the role of caregiving through a wholly compensatory system, a partly compensatory system, and a supportive-educative system. In the wholly compensatory system, the nurse is responsible for the patient’s entire care plan to compensate for the patient’s inability to perform self-care. In the partly compensatory system, both the nurse and the patient participate in self-care. The supportive-educative system is implemented when the patient is ready to learn to perform an activity but is unable to do so without support and education—in this situation, the nurse primarily acts as an educator and advisor [14, 15]. In the present study, the researchers utilized the supportive-educative system defined by Orem’s self-care model.
Given the high prevalence of HTN and its well-established association with life-threatening complications, including myocardial infarction and cerebrovascular accidents, the development and implementation of evidence-based, patient-centered educational strategies are of paramount importance. Most studies in this field have been conducted descriptively, and the few available experimental studies have not utilized Orem’s self-care model. Although previous studies have demonstrated the impact of educational interventions using various models, including Pender’s health promotion model and the health belief model, to enhance the QoL and self-care behaviors of hypertensive patients [16, 17], few studies have investigated the effect of an educational program using Orem’s self-care model in hypertensive patients. Thus, due to the significance of the subject and the limited research conducted in this area, it is recommended that the present study be carried out in different countries to facilitate knowledge translation in patient education. Accordingly, the present study was designed to determine the impact of an educational program using Orem’s self-care model on improving the QoL and health-promoting lifestyle in hypertensive patients in the south of Iran.
Materials and Methods
Study design and sample
This prospective, open-label randomized controlled trial was implemented at two tertiary cardiovascular referral centers located in southern Iran and spanned an eight-month period, from August 2022 to April 2023. Due to the inherently interactive nature of the intervention, blinding of participants and providers was not feasible and therefore was not employed.
The sample size was calculated based on statistical parameters reported by Jamshidi et al. [12], utilizing assumptions appropriate for comparing mean values across two related groups. Assuming a two-tailed significance level (α) of 0.05 and a statistical power (1-β) of 90%, the minimum required sample size for each group was determined to be 28 participants. To account for potential attrition and to enhance the statistical power of the analysis, the sample size was deliberately increased, resulting in the allocation of 40 participants to each group. This adjustment was made to strengthen analytical robustness and improve the generalizability of the study findings.
Inclusion and exclusion criteria were precisely defined to ensure methodological rigor in participant selection. Eligible participants were adults aged between 30 and 55 years with a confirmed clinical diagnosis of HTN who provided written informed consent. Individuals were excluded if they experienced acute clinical deterioration during the study period or voluntarily withdrew their participation at any stage. Such exclusions were applied to preserve the internal validity of the study and to ensure the integrity of the final analysis.
From an initial cohort of 94 individuals diagnosed with HTN, participants were recruited using a non-random convenience sampling method. Following an eligibility assessment based on predefined inclusion criteria, 14 individuals were excluded due to non-compliance with the study’s entry requirements. The final sample comprised 80 participants, who were then randomly assigned to two equal groups: the experimental arm (n=40) and the control arm (n=40).
Random allocation was carried out through a straightforward yet rigorously controlled concealment procedure. Eighty identical cards, with half labeled “A” and the other half labeled “B,” were thoroughly shuffled and placed in a sealed, opaque container to mitigate selection bias. Each eligible participant was instructed to draw a card blindly. Those who selected “A” were assigned to the intervention group, while those who drew “B” were allocated to the control group. A detailed account of participant recruitment, allocation, retention, and follow-up is visually presented in the CONSORT flowchart (Figure 1).
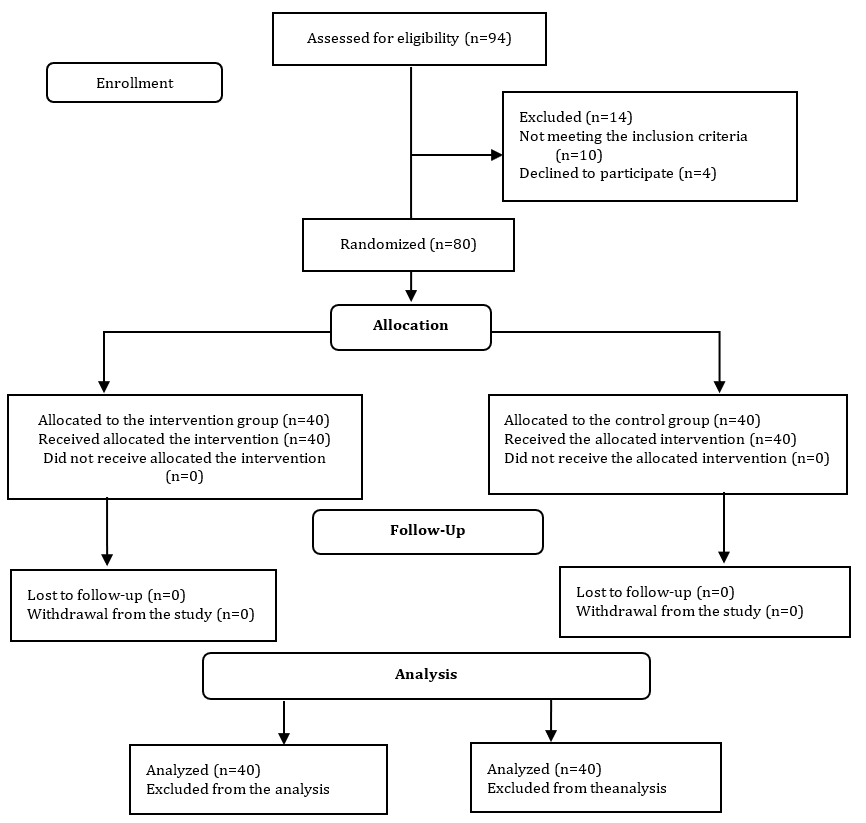
Figure 1. CONSORT flow diagram of the participants throughout the study
Study procedure
Prior to the commencement of the study, full ethical approval was obtained from the Institutional Review Board (IRB) of the affiliated academic institution. Following protocol approval, a formal authorization letter was issued by the Office of the Vice-Chancellor for Research. Upon arrival at the clinical site, the principal investigator provided prospective participants with a clear and comprehensive explanation of the study’s objectives, scope, and procedures. Both verbal and written informed consent were obtained from individuals who agreed to participate.
The educational intervention, meticulously designed in alignment with Dorothea Orem’s self-care theoretical framework, consisted of six structured instructional sessions, each lasting approximately two hours. To preserve group integrity and prevent cross-contamination, sessions were conducted separately for the two groups. Each session accommodated approximately 20 participants, ensuring an optimal facilitator-to-participant ratio conducive to meaningful interaction. The instructional approach incorporated didactic lectures, interactive discussions, and the distribution of printed educational materials. In response to the ongoing COVID-19 pandemic, all sessions strictly adhered to public health guidelines, including physical distancing and routine sanitization.
The educational content was closely aligned with the central tenets of Orem’s model and tailored to address the complex self-care needs of adults managing HTN. Curriculum topics included the physiological mechanisms underlying blood pressure regulation, etiological factors contributing to HTN, and the systemic consequences of uncontrolled blood pressure. Instruction emphasized the development of self-management competencies across several key domains: initiation of regular physical activity, adherence to dietary recommendations, weight management, stress regulation, and engagement in mind-body practices such as diaphragmatic breathing, yoga, and meditation. Additional content focused on risk-reduction behaviors, including smoking cessation, abstinence from alcohol, adherence to prescribed pharmacologic treatments, accurate self-monitoring of blood pressure, and maintenance of routine medical follow-ups.
Each of the six sessions addressed a distinct thematic focus. Session 1 provided an overview of blood pressure physiology, definitions of HTN, and associated health risks; Session 2 explored modifiable and non-modifiable risk factors, along with the long-term complications of poorly controlled HTN; Session 3 introduced the concept of self-care and outlined empirically supported strategies for chronic disease management; Session 4 focused on behavioral lifestyle modifications, including exercise planning, nutritional practices, body weight regulation, and stress coping techniques; Session 5 examined integrative therapies, such as controlled breathing, yoga, and meditation, and addressed the health risks linked to tobacco and alcohol use; and Session 6 featured a hands-on demonstration of home blood pressure monitoring techniques and reinforced the importance of ongoing clinical engagement and medication adherence.
Participants in the intervention group attended all six sessions and had continuous access to expert facilitators who addressed individual questions to ensure thorough comprehension of the material. Printed pamphlets were also provided as supplementary educational resources. In contrast, the control group did not receive any instructional content during the intervention period. However, in accordance with ethical considerations, control participants were given the same informational pamphlets upon completion of the study.
Data collection was conducted at four distinct time points; prior to the intervention (baseline), immediately after the final session, one month following the intervention, and again at the three-month follow-up. At each interval, participants completed validated self-report instruments under the direct supervision of trained research personnel, and blood pressure measurements were performed using standardized clinical procedures.
Prior to participation, all individuals were comprehensively informed about the study’s objectives, methodological procedures, and data usage protocols. Written informed consent was subsequently obtained. Participant confidentiality and anonymity were rigorously preserved throughout the data collection, management, and analysis phases. All procedures adhered strictly to institutional ethical guidelines and the principles outlined in the Declaration of Helsinki. In cases involving legally dependent individuals, informed consent was additionally obtained from authorized legal guardians or representatives.
Instrument
A comprehensive battery of empirically validated tools was employed to facilitate multidimensional data collection. These included a demographic data form, the Short Form-36 Health Survey (SF-36), the Health-Promoting Lifestyle Profile (HPLP), and the Hypertension Self-Care Profile (HTN-SCP), each selected for its established psychometric reliability and direct relevance to the study objectives.
The demographic questionnaire comprised 13 systematically constructed items designed to capture essential sociodemographic and clinical parameters. Collected data included chronological age, gender identity, educational attainment, occupational status, marital status, smoking behavior, systolic and diastolic blood pressure readings, body mass index (BMI), presence of comorbidities, duration since HTN diagnosis, and history of medical consultations related to hypertensive care.
To assess participants’ perceived health-related QoL, the study employed the SF-36, originally developed by Ware & Sherbourne [18]. The Persian-language version, previously translated and psychometrically validated by Montazeri et al. [19], was utilized. This 36-item instrument encompasses eight multidimensional domains, including physical functioning, role limitations due to physical health, role limitations due to emotional problems, vitality, mental health, social functioning, bodily pain, and general health perceptions. Each domain is scored on a scale from 0 to 100, with higher scores reflecting better perceived health status and overall QoL.
Lifestyle behaviors associated with sustained health promotion were evaluated using the Health-Promoting Lifestyle Profile (HPLP), originally developed by Walker & Hill-Polerecky [20]. This instrument measures six critical dimensions of health behavior, including nutrition, physical activity, health responsibility, interpersonal relations, stress management, and self-actualization. Its Persian version, psychometrically validated by Mohammadi Zeidi et al. [21], comprises 52 items rated on a four-point Likert scale ranging from 1 (never) to 4 (routinely). Cumulative scores indicate the extent to which individuals engage in behaviors conducive to health promotion.
HTN-specific self-care competencies were assessed using the Hypertension Self-Care Profile (HTN-SCP), developed by Han et al. [22]. Although initially validated among Korean American populations, the instrument was later culturally adapted and validated for use among Iranian adults by Mohammadnejad et al. [23]. The HTN-SCP consists of 20 items spanning four principal domains: adherence to dietary and exercise recommendations, compliance with prescribed medications, ability to interpret nutritional labels, and general self-management of HTN. Each item employs a four-point response scale, with higher scores indicating greater adherence to recommended self-care behaviors.
Statistical analysis
Data analyses were conducted using SPSS 22. Between-group differences were assessed using independent sample t-tests for continuous parameters and Chi-square tests for categorical parameters. To examine within-group changes over time, repeated measures analysis of variance (ANOVA) was employed, allowing for the longitudinal evaluation of intervention effects across multiple time points.
Findings
The final analytical sample comprised 80 adult participants with a confirmed diagnosis of HTN, with a mean age of 44.16±4.60 years. The mean age in the control and intervention groups was 44.80±5.09 and 43.53±4.13 years, respectively (p=0.222). Baseline demographic characteristics showed no statistically significant differences between the experimental and control groups, thereby confirming the initial comparability of the cohorts. Similarly, pre-intervention QoL scores did not exhibit any meaningful intergroup differences (Table 1).
Table 1. Demographic information of the subjects
Post-intervention assessments, however, revealed statistically significant improvements in QoL among participants in the educational intervention group. These enhancements were sustained at both the one-month and three-month follow-up assessments compared to the control group (p<0.001; Table 2).
Table 2. Comparing the mean quality of life scores in the groups before and after the educational intervention
Although no significant differences in health-promoting lifestyle behaviors were observed at baseline, the intervention group demonstrated substantial and statistically significant improvements across all post-intervention time points (p<0.001; Table 3).
Table 3. Comparing the mean lifestyle scores in the groups before and after the intervention
A similar pattern emerged in the domain of self-care efficacy. Baseline scores did not differ significantly between the two groups; however, participants in the intervention group exhibited marked improvements following the intervention. These gains remained statistically robust at both follow-up intervals (p<0.001; Table 4).
Table 4. Comparing the mean self-care scores in the groups before and after the intervention
Regarding blood pressure outcomes, baseline systolic and diastolic values were statistically comparable between the groups. Notably, the intervention group experienced a significant reduction in systolic blood pressure immediately post-intervention and at the one-month follow-up. Although this reduction diminished slightly by the three-month evaluation, diastolic blood pressure levels in the intervention group continued to demonstrate statistically significant and clinically meaningful reductions across all follow-up time points (p<0.001; Table 5).
Table 5. Comparing the mean scores of systolic and diastolic blood pressures in the groups before and after the intervention
Discussion
This study systematically evaluated the effectiveness of a theory-driven self-care educational intervention, grounded in Orem’s conceptual model, in enhancing QoL and fostering health-promoting behaviors among individuals diagnosed with HTN. The equivalence of baseline characteristics across study arms served to strengthen the internal validity of the observed outcomes.
Following the implementation of the six-session instructional program, participants in the intervention group exhibited statistically significant improvements in both subjective well-being and self-regulatory health behaviors. While reductions in systolic blood pressure were apparent immediately post-intervention and at the one-month follow-up, this trend attenuated somewhat by the third month, suggesting a potential need for periodic reinforcement. In contrast, diastolic pressure reductions remained stable and statistically significant throughout the follow-up period, indicating a more durable physiological response to the intervention.
These findings are congruent with those of Bairami et al., reporting a strong association between active self-care engagement and improved QoL among individuals with chronic conditions. The current study extends this line of inquiry by providing additional empirical support for the efficacy of structured educational programs, particularly when underpinned by a well-established nursing theory. The results confirm that theoretically guided interventions can produce sustained improvements in both behavioral and clinical outcomes in hypertensive populations [24].
A substantial body of empirical research has underscored the critical role of lifestyle modification in optimizing clinical outcomes among individuals with chronic diseases. In a descriptive-comparative study, Zareei et al. demonstrate a clear and direct relationship between positive behavioral changes and enhanced health indices [25]. Consistent with this body of evidence, the present study documented significant improvements across multiple lifestyle dimensions following the implementation of a targeted self-care training program. Concurrent reductions in systolic and diastolic blood pressure provided further validation of the intervention’s effectiveness in mitigating cardiovascular risk.
Similar conclusions were drawn by Asa Kohneforoudi et al., who found that adherence to self-care practices significantly predicts higher levels of self-efficacy, a recognized psychosocial determinant of successful HTN prevention and management [26]. Their endorsement of individualized, behaviorally oriented interventions is reflected in the current study’s application of Orem’s theoretical framework, which informed the design of a personalized educational strategy. This model-based approach yielded measurable benefits in both cognitive-behavioral and physiological domains, thereby reinforcing its practical relevance and applicability in clinical settings.
Further empirical support for comprehensive self-management strategies was provided by Arabshahi et al., identifying a notable adherence gap, particularly regarding sodium restriction, despite relatively high compliance with medication use and physical activity guidelines. They reported that approximately 25% of patients are unable to effectively limit dietary sodium intake [27]. In alignment with these findings, the present intervention adopted a holistic perspective by integrating key components of HTN management, including nutritional modification, pharmacologic adherence, and physical activity promotion. This multidimensional approach contributed to significant and sustained reductions in both systolic and diastolic blood pressure, underscoring the necessity of comprehensive self-care education.
In a cross-national investigation conducted across three healthcare institutions in Sri Lanka, Pirasath et al. have identified widespread deficits in patient awareness concerning diagnostic criteria, treatment goals, and personal blood pressure targets, despite a general understanding of HTN risk factors. Although in the mentioned study, medication adherence is rated as satisfactory, memory lapses frequently is emerged as a principal barrier to consistent therapeutic compliance. In response, the authors have advocated for the implementation of individualized educational interventions [28]. Echoing this recommendation, the current study incorporated modular instruction covering key topics, such as the pathophysiology of HTN, potential complications, pharmacologic adherence, and the importance of regular medical follow-up. The observed improvements in patient-reported outcomes following the intervention provide compelling evidence for the efficacy of this educational model.
Ketata et al. report a constellation of risk factors associated with suboptimal self-care engagement, including advanced disease severity, the presence of comorbid respiratory conditions, limited formal education, and the absence of prior instruction in self-management strategies [29]. These findings highlight the importance of tailoring health education to reflect the sociodemographic and clinical profiles of target populations. Within this context, the present study’s implementation of a theory-informed, demographically sensitive intervention significantly enhanced participants’ self-care capabilities, thereby demonstrating its effectiveness in addressing diverse patient needs.
The critical importance of non-pharmacologic strategies in the management of HTN was reaffirmed by Carey et al., whose comprehensive guideline review positions lifestyle modification as the cornerstone of effective blood pressure control [30]. Their recommendations highlight several key behavioral targets, including dietary moderation (specifically, sodium reduction and potassium enrichment), balanced nutritional intake, routine physical activity, and responsible alcohol consumption. The empirical findings of the present study align closely with these best-practice recommendations. Participants in the intervention group demonstrated improved adherence to prescribed lifestyle modifications, which corresponded with statistically significant reductions in both systolic and diastolic blood pressure. These results suggest a synergistic relationship between enhancements in QoL and positive lifestyle behavioral changes, collectively contributing to sustained blood pressure regulation.
The participants were recruited from a single center in southern Iran, which may limit the generalizability of the findings. Another limitation of this study was the small sample size; it is recommended to use a larger population size in similar research. Additionally, the lack of blinding and the non-equivalent intervention intensity between groups, as well as the short time period between the intervention and the assessment of the patients’ outcomes, can be mentioned as limitations. It is further suggested that longitudinal and prospective cohort studies be conducted. Data were collected using self-reported measures such as self-efficacy and life satisfaction scores. Potential response bias may have resulted from participants providing answers they perceived as socially acceptable or that did not accurately represent their genuine emotions and experiences.
It is recommended that periodic booster sessions or continuous support mechanisms be instituted to maintain behavioral momentum, facilitate enduring lifestyle adjustments, and promote long-term hemodynamic stability.
Conclusion
The Orem-based self-care educational intervention leads to meaningful short-term improvements in QoL and health-promoting behaviors among individuals with HTN.
Acknowledgments: The authors express their sincere appreciation to the emergency medical personnel whose active participation and cooperation were instrumental to the successful execution of the study. The authors also extend special thanks to Fasa University of Medical Sciences for institutional support and to the Clinical Research Development Unit of Fasa Valiasr Hospital for their invaluable assistance with logistical coordination and financial oversight.
Ethical Permissions: The study protocol received ethical clearance from the Research Ethics Committee of Fasa University of Medical Sciences (Approval No. IR.FUMS.REC.1400.153), and all procedures adhered strictly to institutional ethical guidelines and the principles outlined in the Declaration of Helsinki. IRCT Registration Number: IRCT20190917044802N4.
Conflicts of Interests: The authors declared no conflicts of interests.
Authors' Contribution: Kouhi F (First Author), Methodologist/Assistant Researcher/Discussion Writer/Statistical Analyst (25%); Bijani M (Second Author), Introduction Writer/Methodologist/Main Assistant Researcher/Discussion Writer (35%); Fereidouni Zh (Third Author), Methodologist/Assistant Researcher/Statistical Analyst (30%); Dehghan A (Fourth Author), Introduction Writer/Methodologist/ Assistant Researcher (5%); Taghinezhad A (Fifth Author), Assistant Researcher/Discussion Writer/Statistical Analyst (5%)
Funding/Support: This research was conducted independently and did not receive funding from governmental agencies, commercial enterprises, or nonprofit organizations.
Keywords:
References
1. Oparil S, Acelajado MC, Bakris GL, Berlowitz DR, Cífková R, Dominiczak AF, et al. Hypertension. Nat Rev Dis Primers. 2018;4(1):18014. [Link] [DOI:10.1038/nrdp.2018.14]
2. Mills KT, Stefanescu A, He J. The global epidemiology of hypertension. Nat Rev Nephrol. 2020;16(4):223-37. [Link] [DOI:10.1038/s41581-019-0244-2]
3. Adamu K, Feleke A, Muche A, Yasin T, Mekonen AM, Chane MG, et al. Health related quality of life among adult hypertensive patients on treatment in Dessie city, Northeast Ethiopia. PLoS One. 2022;17(9):e0268150. [Link] [DOI:10.1371/journal.pone.0268150]
4. Egan BM, Kjeldsen SE, Grassi G, Esler M, Mancia G. The global burden of hypertension exceeds 1.4 billion people: Should a systolic blood pressure target below 130 become the universal standard?. J Hypertens. 2019;37(6):1148-53. [Link] [DOI:10.1097/HJH.0000000000002021]
5. Gheirati Ghasem Abadi A, Mousavi Bazaz M. Quality of life and its related factors in hypertensive patients. J North Khorasan Univ Med Sci. 2020;12(2):80-7. [Persian] [Link] [DOI:10.52547/nkums.12.2.80]
6. Bijani M, Khaleghi AA, Hatami M, Najafi H, Haghshenas A. A study of the consistency between hypertension medications prescribed by general practitioners and 2018 ESC/ESH guidelines for the management of hypertension. REVISTA LATINOAMERICANA DE HIPERTENSION. 2019;14(1):32-6. [Link]
7. Malekzadeh MM, Etemadi A, Kamangar F, Khademi H, Golozar A, Islami F, et al. Prevalence, awareness and risk factors of hypertension in a large cohort of Iranian adult population. J Hypertens. 2013;31(7):1364-71. [Link] [DOI:10.1097/HJH.0b013e3283613053]
8. Bijani M, Parvizi S, Dehghan A, Sedigh-Rahimabadi M, Rostami-Chijan M, Kazemi M, et al. Investigating the prevalence of hypertension and its associated risk factors in a population-based study: Fasa PERSIAN COHORT data. BMC Cardiovasc Disord. 2020;20(1):503. [Link] [DOI:10.1186/s12872-020-01797-3]
9. Najafi Ghezeljeh T, Shahidi M. Self-care education and improving quality of life in patients with hypertension: A review literature. Iran J Cardiovasc Nurs. 2014;3(1):66-71. [Persian] [Link]
10. Baghi V, Baghban Karimi E. Predicting the quality of life of patients with hypertension based on resilience and social support. Iran J Psychiatr Nurs. 2018;5(6):24-30. [Persian] [Link] [DOI:10.21859/ijpn-05064]
11. Nasresabetghadam S, Jahanshahi M, Fotokian Z, Nasiri M, Hajiahmadi M. The effects of Orem's self-care theory on self-care behaviors among older women with hypertension: A randomized controlled trial. Nurs Midwifery Stud. 2021;10(2):99-106. [Link] [DOI:10.4103/nms.nms_9_20]
12. Jamshidi A, Rozbahani N, Nasirian M. The effect of group discussion on self-care behaviors among hypertensive patients referring to health care centers in Arak City. Sci J Kurdistan Univ Med Sci. 2019;24(5):56-68. [Persian] [Link] [DOI:10.29252/sjku.24.5.56]
13. Shah M, Abdullah A, Khan H. Compare and contrast of grand theories: Orem's self-care deficit theory and Roy's adaptation model. Int J Sci Res. 2015;4(1):1834-7. [Link]
14. Valizadeh S, Soheili A, Moghbeli G, Aliafsari E. Applicablity of Orem's self-care model in Iran: An integrated review. Nurs Midwifery J. 2017;15(4):313-28. [Persian] [Link]
15. Aligood MR. Nursing theorists and their works. 9th ed. New York: Elsevier; 2017. [Link]
16. Taghadosi M, Nouri H. The effect of education based on "pender health promotion model" on adherence to treatment of patients with hypertension. J Health Promot Manag. 2023;12(1):69-80. [Persian] [Link]
17. Kasmaei P, Yousefi P, Farmanbar R, Omidi S, Karimy M, Bab Eghbal S, et al. The impact of health belief model-based education on self-care behaviors of hypertensive patients. Casp J Health Res. 2024;9(4):237-48. [Link] [DOI:10.32598/CJHR.9.4.1916.1]
18. Ware JE, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30(6):473-83. [Link] [DOI:10.1097/00005650-199206000-00002]
19. Montazeri A, Gashtasbi A, Vahdaninia MB. The short form health survey (SF-36): Translation and validation study of the Iranian version. PAYESH. 2006;5(1):49-56. [Persian] [Link]
20. Walker SN, Hill-Polerecky DM. Psychometric evaluation of health promoting lifestyle profile II. Unpublished manuscript. Nebraska: University of Nebraska Medical Center; 1997. [Link]
21. Mohammadi Zeidi I, Pakpour Hajiagha A, Mohammadi Zeidi B. Reliability and validity of Persian version of the health-promoting lifestyle profile. J Mazandaran Univ Med Sci. 2011;20(1):102-13. [Persian] [Link]
22. Han HR, Song HJ, Nguyen T, Kim MT. Measuring self-care in patients with hypertension: A systematic review of literature. J Cardiovasc Nurs. 2014;29(1):55-67. [Link] [DOI:10.1097/JCN.0b013e3182775fd1]
23. Mohammadnejad E, Seifi A, Ghanei Gheshlagh R, Aliramezani A, Fattah Ghazi S, Salehi M, et al. Determine phenotypical patterns of resistance to antibiotics in COVID-19 patients with associated bacterial infection: Largest medical center in Iran. Iran J Microbiol. 2023;15(3):336-42. [Link] [DOI:10.18502/ijm.v15i3.12893]
24. Bairami S, Fathi Y, Mohammadinasab S, Barati M, Mohammadi Y. Relationship between self-care behaviors and quality of life among hypertensive patients visiting comprehensive health centers in Hamadan, Iran. J Educ Community Health. 2017;4(1):20-7. [Persian] [Link] [DOI:10.21859/jech.4.1.20]
25. Zareei F, Karimi Jaberi M, Mohsseni SH, Velayati M, Nasari M, Amiri F, et al. Lifestyle of people with hypertension: A case-control study. J Prevent Med. 2021;8(1):58-69. [Persian] [Link] [DOI:10.52547/jpm.8.1.69]
26. Asa Kohneforoudi Z, Gholian-Aval M, Tehrani H, Esmaily H. Evaluation of self-care status and its relationship with self-efficacy of patients with hypertension. Iran J Health Educ Health Promot. 2021;8(4):336-47. [Persian] [Link] [DOI:10.29252/ijhehp.8.4.336]
27. Arabshahi A, Gharlipour Z, Hossein Alipour SA, Mohebi S. Assessment of adherence to self-care behaviors in hypertensive patients in Qom City (Iran). Qom Univ Med Sci J. 2020;14(2):55-66. [Persian] [Link] [DOI:10.29252/qums.14.2.55]
28. Pirasath S, Sugathapala AGH, Wanigasuriya K. Descriptive cross-sectional study on knowledge, awareness, and adherence to medication among hypertensive patients at a tertiary care centre in Colombo district, Sri Lanka. Int J Hypertens. 2020;2020:1320109. [Link] [DOI:10.1155/2020/1320109]
29. Ketata N, Ben Ayed H, Ben Hmida M, Abdelhedi Z, Ben Jemaa M, Trigui M, et al. Prevalence and predictors of hypertension self-care practice in primary health-care facilities in Southern Tunisia. J Med Vasc. 2021;46(2):72-9. [Link] [DOI:10.1016/j.jdmv.2021.01.005]
30. Carey RM, Moran AE, Whelton PK. Treatment of hypertension: A review. JAMA. 2022;328(18):1849-61. [Link] [DOI:10.1001/jama.2022.19590]