Volume 6, Issue 4 (2025)
J Clinic Care Skill 2025, 6(4): 233-236 |
Back to browse issues page
Article Type:
Subject:
History
Received: 2025/08/6 | Accepted: 2025/09/13 | Published: 2025/09/25
Received: 2025/08/6 | Accepted: 2025/09/13 | Published: 2025/09/25
How to cite this article
Alizadeh Z, Zadehbagheri F, Jokar S. Persistent Hypotension with Relative Bradycardia After Surgery; An Unusual Case of Preventable Hypothermic Shock. J Clinic Care Skill 2025; 6 (4) :233-236
URL: http://jccs.yums.ac.ir/article-1-444-en.html
URL: http://jccs.yums.ac.ir/article-1-444-en.html
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



Rights and permissions
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
1- Department of Anesthesiology, Faculty of Medicine, Yasuj University of Medical Sciences, Yasuj, Iran
2- Department of Cardiology, Faculty of Medicine, Yasuj University of Medical Sciences, Yasuj, Iran
3- Department of Internal Medicine, Faculty of Medicine, Yasuj University of Medical Sciences, Yasuj, Iran
2- Department of Cardiology, Faculty of Medicine, Yasuj University of Medical Sciences, Yasuj, Iran
3- Department of Internal Medicine, Faculty of Medicine, Yasuj University of Medical Sciences, Yasuj, Iran
Full-Text (HTML) (2 Views)
Introduction
Hypotension in the postoperative period is a common and potentially life-threatening event that warrants immediate evaluation and targeted management. In most cases, the hemodynamic response to shock—whether hypovolemic, distributive, or cardiogenic—is characterized by compensatory tachycardia [1, 2]. However, the presence of hypotension accompanied by relative bradycardia is uncommon and often signals a distinct pathophysiological mechanism. This presentation may be associated with conditions, such as high-grade atrioventricular block, medication effects (e.g., beta-blockers, calcium channel blockers), electrolyte disturbances, spinal or neuraxial anesthesia-related complications, or hypothermia [3-6].
Failure to promptly identify the underlying cause can delay definitive treatment and lead to adverse outcomes [7, 8]. This is particularly important in the perioperative setting, where environmental factors, procedural complications, and patient-specific vulnerabilities may interact in unexpected ways [9-11].
We presented a case of persistent postoperative hypotension with relative bradycardia that was unresponsive to aggressive fluid resuscitation and standard initial measures. The etiology was traced to an unusual but entirely preventable cause—perioperative hypothermia due to a wet surgical drape. This case underscores the need for a broad differential diagnosis in atypical shock presentations and highlights the importance of thorough physical and environmental assessments in postoperative care [5, 12, 13].
Patients and Methods
A 54-year-old woman with a history of a large uterine fibroid underwent a total abdominal hysterectomy (TAH) under general anesthesia. The procedure was completed uneventfully, and the patient was transferred to the recovery room. Shortly after her arrival, she developed severe hypotension that persisted for approximately 40 minutes (BP: 70/40mmHg) with a relatively low heart rate (PR: 55bpm). Her core body temperature was recorded at 35.3°C, indicating hypothermia.
Findings
On physical examination, the patient exhibited cold, clammy skin. Lung auscultation was clear, and cardiac examination revealed normal heart sounds without murmurs or gallops. Laboratory investigations were unremarkable, including a normal complete blood count (white blood cells (WBCs): 8,100/mm³, hemoglobin (Hb): 13.8g/dL, platelets (Plt): 189×10³/mm³). Arterial blood gas analysis showed pH: 7.33, PCO₂: 35mmHg, HCO₃⁻: 20mmol/L, and base excess (BE): -4. Cardiac biomarkers (troponin) were negative.
Electrocardiography revealed sinus rhythm with relative bradycardia. Transthoracic echocardiography demonstrated a left ventricular ejection fraction of 55%, a pulmonary artery pressure of 18mmHg, normal right ventricular function, and no valvular abnormalities. Urinalysis was unremarkable. There was no clinical or laboratory evidence of active bleeding, infection, or electrolyte disturbances.
Despite the rapid intravenous infusion of approximately 2 liters of normal saline, the hemodynamic parameters did not improve. Upon further thorough physical and environmental assessment, a wet green surgical drape was found underneath the patient’s back, causing heat loss through conduction and evaporation. The drape was immediately removed, and the patient was actively rewarmed using blankets and a warming device.
Following the removal of the wet drape, her vital signs improved significantly (blood pressure (BP): 110/70mmHg, pulse rate (PR): 75bpm, temperature: 36.3°C). During subsequent inpatient monitoring, she remained hemodynamically stable (BP: 110/80mmHg, temperature: 36.9°C) without further complications until discharge (Table 1 and Figure 1).
Table 1. Vital sign trends before and after the intervention
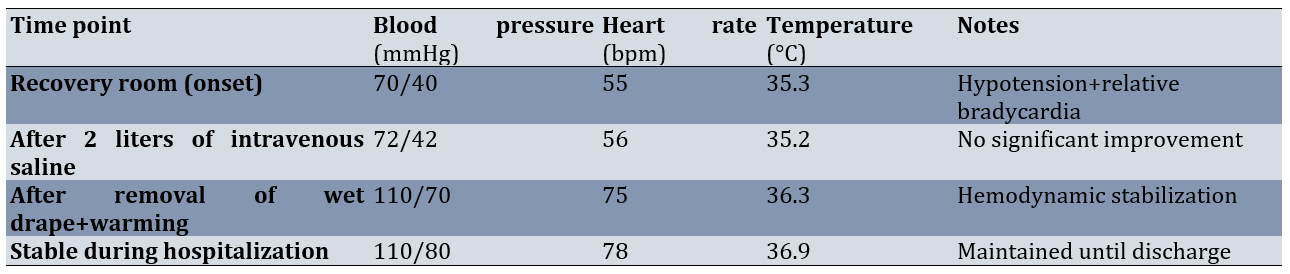
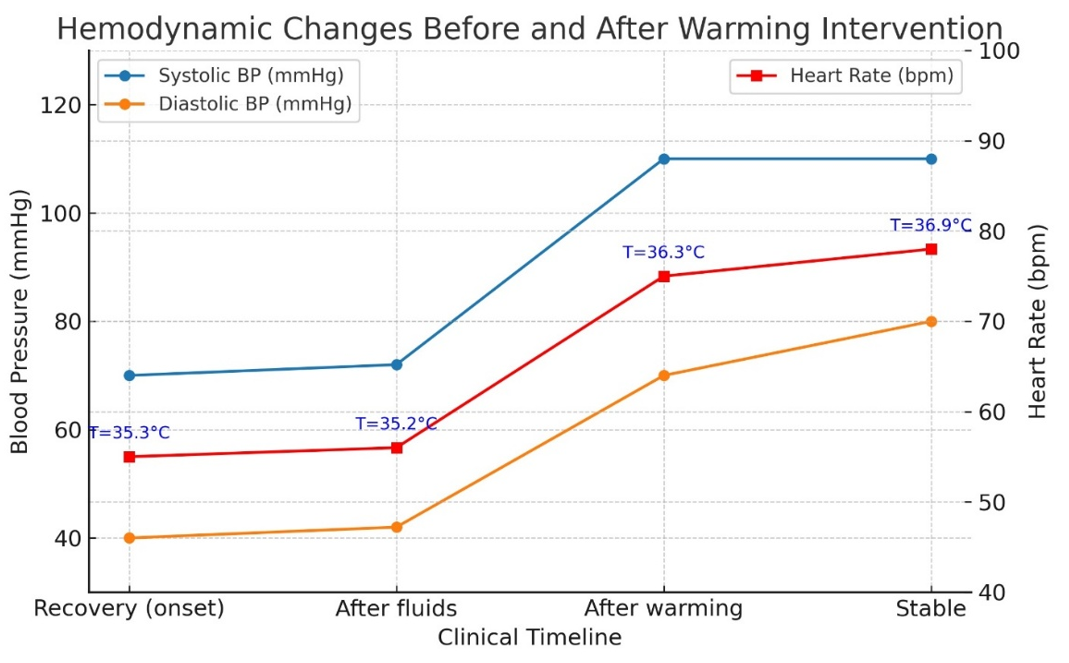
Figure 1. Hemodynamic changes before and after warming intervention.
Systolic and diastolic blood pressure (left y-axis) and heart rate (right y-axis) were plotted across the clinical timeline. Core body temperature at each time point is shown as annotations. Despite fluid resuscitation, hypotension with relative bradycardia persisted until the removal of the wet drape and active rewarming, after which hemodynamic stability was restored and maintained throughout hospitalization.
Discussion
Postoperative hypotension is most often attributed to hypovolemia, sepsis, myocardial dysfunction, or vasodilation due to anesthetic agents, and the physiological response typically involves compensatory tachycardia mediated by sympathetic activation [1, 2]. The occurrence of hypotension with relative bradycardia is atypical and narrows the differential diagnosis to specific conditions such as high-grade atrioventricular block, medication-induced bradycardia (e.g., dexmedetomidine, beta-blockers, calcium channel blockers), electrolyte disturbances, spinal shock, severe intracranial pathology, and hypothermia [1, 2, 13].
In our case, common causes were systematically excluded: the patient had normal cardiac function on echocardiography, no ischemic changes on the ECG, negative troponin, normal laboratory findings, and no evidence of active bleeding, infection, or electrolyte imbalance. Despite aggressive intravenous fluid resuscitation, hypotension persisted, suggesting a non-volume-related mechanism.
Hypothermia is a well-recognized but sometimes overlooked cause of postoperative hemodynamic instability [2-5]. It exerts its effects through several mechanisms. First, cardiac conduction slowing occurs because lower core temperatures decrease the pacemaker cell depolarization rate, leading to sinus bradycardia [1, 2]. Second, hypothermia reduces myocardial contractility due to impaired calcium handling and cross-bridge cycling [1]. Third, it causes peripheral vasodilation, including paradoxical vasodilation during rewarming, which reduces systemic vascular resistance [1, 3]. Finally, hypothermia impairs catecholamine responsiveness, resulting in blunted adrenergic receptor sensitivity and limiting compensatory tachycardia [1, 3].
The persistence of hypotension with bradycardia in our patient was ultimately explained by inadvertent prolonged contact with a wet surgical drape, resulting in heat loss through conduction and evaporation. The removal of the wet drape and active rewarming promptly restored hemodynamic stability, underscoring the reversibility of hypothermia-induced cardiovascular depression when recognized promptly [2, 3, 11, 12].
This case reinforces several important clinical lessons. First, in postoperative shock with relative bradycardia, hypothermia should be considered early in the differential diagnosis, especially when standard causes are excluded [2, 5, 11]. Second, a thorough environmental and physical assessment is essential in critically ill or unstable patients to identify preventable sources of heat loss [2, 3]. Third, preventable perioperative factors (such as inadequate thermal insulation or retained wet materials) should be addressed within surgical safety and warming protocols, given the established links between inadvertent hypothermia and adverse outcomes, including delayed recovery, increased blood loss/transfusion, and surgical-site infection [1-3, 9, 10, 14].
Our experience aligns with prior reports emphasizing the importance of continuous perioperative temperature monitoring, proactive warming strategies, and vigilance against environmental heat loss to improve patient safety and outcomes [1, 2, 5, 9, 10, 14].
This case illustrates an uncommon presentation of postoperative shock characterized by persistent hypotension with relative bradycardia, ultimately caused by an entirely preventable environmental factor—perioperative hypothermia from a wet surgical drape. The absence of typical compensatory tachycardia should prompt clinicians to broaden their differential diagnosis beyond common causes such as hypovolemia and sepsis. Systematic evaluation, including environmental and physical assessments, is crucial when standard investigations are unrevealing. Early recognition and correction of hypothermia can rapidly restore hemodynamic stability and prevent unnecessary interventions.
Hypotension with relative bradycardia in the postoperative period is uncommon and should prompt consideration of specific causes such as hypothermia, conduction disturbances, or medication effects. Hypothermia can lead to reversible cardiovascular depression by inducing bradycardia, reducing myocardial contractility, and impairing vascular tone. Environmental and physical factors must be systematically assessed in unstable postoperative patients, especially when the initial diagnostic workup is unrevealing.
Perioperative hypothermia is preventable through appropriate patient warming strategies, avoidance of prolonged exposure to cold surfaces, and vigilance against retained wet materials. Early identification and intervention can rapidly reverse hypothermia-induced instability, thereby avoiding unnecessary invasive procedures and improving patient safety.
Conclusion
Perioperative hypothermia is preventable through appropriate patient warming strategies, avoidance of prolonged exposure to cold surfaces, and vigilance against retained wet materials.
Acknowledgments: We thank the patient for consenting to publication and the medical team for their support. We also express our sincere gratitude to Dr. Zahra Hosseini for her valuable assistance in finalizing the manuscript.
Ethical Permissions: Written informed consent was obtained from the patient.
Conflicts of Interests: The authors declared no conflicts of interests.
Authors' Contribution: Alizadeh Z (First Author), Introduction Writer/Methodologist/Assistant Researcher/Discussion Writer/Statistical Analyst (30%); Zadehbagheri F (Second Author), Researcher/Discussion Writer/Statistical Analyst (25%); Jokar S (Third Author), Introduction Writer/Methodologist/Main Researcher/Discussion Writer (45%)
Funding/Support: No funding or financial support was received.
Hypotension in the postoperative period is a common and potentially life-threatening event that warrants immediate evaluation and targeted management. In most cases, the hemodynamic response to shock—whether hypovolemic, distributive, or cardiogenic—is characterized by compensatory tachycardia [1, 2]. However, the presence of hypotension accompanied by relative bradycardia is uncommon and often signals a distinct pathophysiological mechanism. This presentation may be associated with conditions, such as high-grade atrioventricular block, medication effects (e.g., beta-blockers, calcium channel blockers), electrolyte disturbances, spinal or neuraxial anesthesia-related complications, or hypothermia [3-6].
Failure to promptly identify the underlying cause can delay definitive treatment and lead to adverse outcomes [7, 8]. This is particularly important in the perioperative setting, where environmental factors, procedural complications, and patient-specific vulnerabilities may interact in unexpected ways [9-11].
We presented a case of persistent postoperative hypotension with relative bradycardia that was unresponsive to aggressive fluid resuscitation and standard initial measures. The etiology was traced to an unusual but entirely preventable cause—perioperative hypothermia due to a wet surgical drape. This case underscores the need for a broad differential diagnosis in atypical shock presentations and highlights the importance of thorough physical and environmental assessments in postoperative care [5, 12, 13].
Patients and Methods
A 54-year-old woman with a history of a large uterine fibroid underwent a total abdominal hysterectomy (TAH) under general anesthesia. The procedure was completed uneventfully, and the patient was transferred to the recovery room. Shortly after her arrival, she developed severe hypotension that persisted for approximately 40 minutes (BP: 70/40mmHg) with a relatively low heart rate (PR: 55bpm). Her core body temperature was recorded at 35.3°C, indicating hypothermia.
Findings
On physical examination, the patient exhibited cold, clammy skin. Lung auscultation was clear, and cardiac examination revealed normal heart sounds without murmurs or gallops. Laboratory investigations were unremarkable, including a normal complete blood count (white blood cells (WBCs): 8,100/mm³, hemoglobin (Hb): 13.8g/dL, platelets (Plt): 189×10³/mm³). Arterial blood gas analysis showed pH: 7.33, PCO₂: 35mmHg, HCO₃⁻: 20mmol/L, and base excess (BE): -4. Cardiac biomarkers (troponin) were negative.
Electrocardiography revealed sinus rhythm with relative bradycardia. Transthoracic echocardiography demonstrated a left ventricular ejection fraction of 55%, a pulmonary artery pressure of 18mmHg, normal right ventricular function, and no valvular abnormalities. Urinalysis was unremarkable. There was no clinical or laboratory evidence of active bleeding, infection, or electrolyte disturbances.
Despite the rapid intravenous infusion of approximately 2 liters of normal saline, the hemodynamic parameters did not improve. Upon further thorough physical and environmental assessment, a wet green surgical drape was found underneath the patient’s back, causing heat loss through conduction and evaporation. The drape was immediately removed, and the patient was actively rewarmed using blankets and a warming device.
Following the removal of the wet drape, her vital signs improved significantly (blood pressure (BP): 110/70mmHg, pulse rate (PR): 75bpm, temperature: 36.3°C). During subsequent inpatient monitoring, she remained hemodynamically stable (BP: 110/80mmHg, temperature: 36.9°C) without further complications until discharge (Table 1 and Figure 1).
Table 1. Vital sign trends before and after the intervention
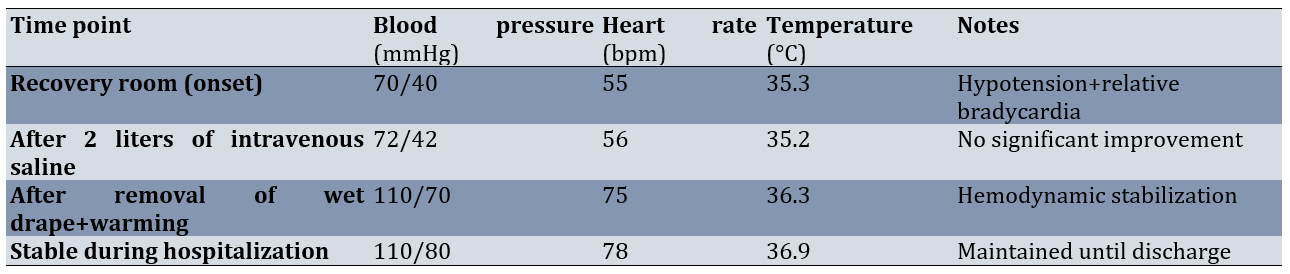
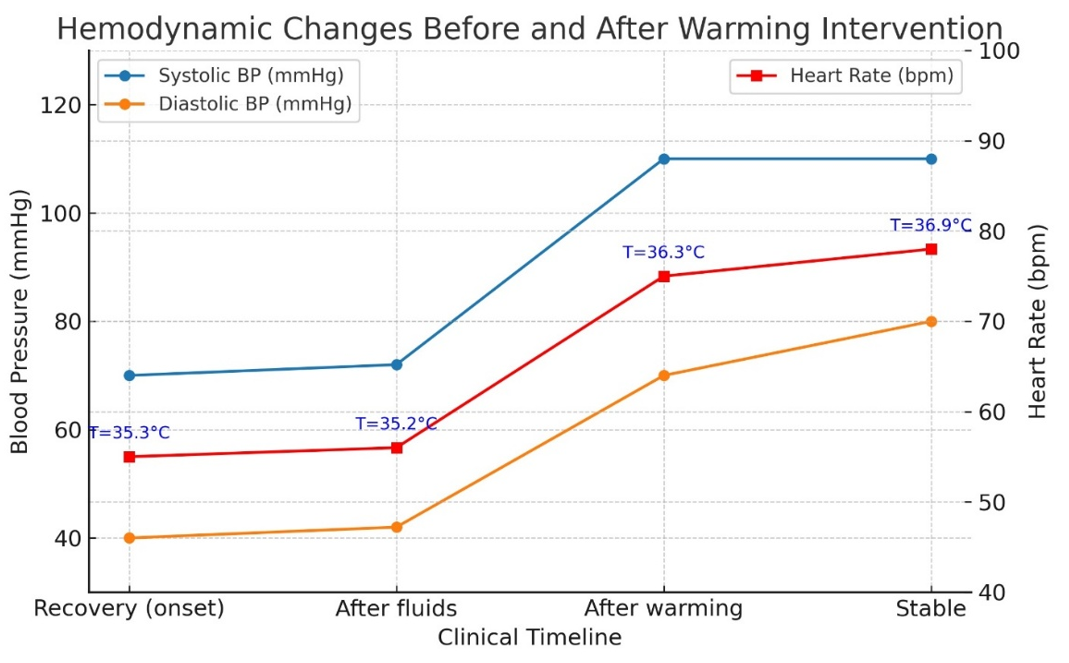
Figure 1. Hemodynamic changes before and after warming intervention.
Systolic and diastolic blood pressure (left y-axis) and heart rate (right y-axis) were plotted across the clinical timeline. Core body temperature at each time point is shown as annotations. Despite fluid resuscitation, hypotension with relative bradycardia persisted until the removal of the wet drape and active rewarming, after which hemodynamic stability was restored and maintained throughout hospitalization.
Discussion
Postoperative hypotension is most often attributed to hypovolemia, sepsis, myocardial dysfunction, or vasodilation due to anesthetic agents, and the physiological response typically involves compensatory tachycardia mediated by sympathetic activation [1, 2]. The occurrence of hypotension with relative bradycardia is atypical and narrows the differential diagnosis to specific conditions such as high-grade atrioventricular block, medication-induced bradycardia (e.g., dexmedetomidine, beta-blockers, calcium channel blockers), electrolyte disturbances, spinal shock, severe intracranial pathology, and hypothermia [1, 2, 13].
In our case, common causes were systematically excluded: the patient had normal cardiac function on echocardiography, no ischemic changes on the ECG, negative troponin, normal laboratory findings, and no evidence of active bleeding, infection, or electrolyte imbalance. Despite aggressive intravenous fluid resuscitation, hypotension persisted, suggesting a non-volume-related mechanism.
Hypothermia is a well-recognized but sometimes overlooked cause of postoperative hemodynamic instability [2-5]. It exerts its effects through several mechanisms. First, cardiac conduction slowing occurs because lower core temperatures decrease the pacemaker cell depolarization rate, leading to sinus bradycardia [1, 2]. Second, hypothermia reduces myocardial contractility due to impaired calcium handling and cross-bridge cycling [1]. Third, it causes peripheral vasodilation, including paradoxical vasodilation during rewarming, which reduces systemic vascular resistance [1, 3]. Finally, hypothermia impairs catecholamine responsiveness, resulting in blunted adrenergic receptor sensitivity and limiting compensatory tachycardia [1, 3].
The persistence of hypotension with bradycardia in our patient was ultimately explained by inadvertent prolonged contact with a wet surgical drape, resulting in heat loss through conduction and evaporation. The removal of the wet drape and active rewarming promptly restored hemodynamic stability, underscoring the reversibility of hypothermia-induced cardiovascular depression when recognized promptly [2, 3, 11, 12].
This case reinforces several important clinical lessons. First, in postoperative shock with relative bradycardia, hypothermia should be considered early in the differential diagnosis, especially when standard causes are excluded [2, 5, 11]. Second, a thorough environmental and physical assessment is essential in critically ill or unstable patients to identify preventable sources of heat loss [2, 3]. Third, preventable perioperative factors (such as inadequate thermal insulation or retained wet materials) should be addressed within surgical safety and warming protocols, given the established links between inadvertent hypothermia and adverse outcomes, including delayed recovery, increased blood loss/transfusion, and surgical-site infection [1-3, 9, 10, 14].
Our experience aligns with prior reports emphasizing the importance of continuous perioperative temperature monitoring, proactive warming strategies, and vigilance against environmental heat loss to improve patient safety and outcomes [1, 2, 5, 9, 10, 14].
This case illustrates an uncommon presentation of postoperative shock characterized by persistent hypotension with relative bradycardia, ultimately caused by an entirely preventable environmental factor—perioperative hypothermia from a wet surgical drape. The absence of typical compensatory tachycardia should prompt clinicians to broaden their differential diagnosis beyond common causes such as hypovolemia and sepsis. Systematic evaluation, including environmental and physical assessments, is crucial when standard investigations are unrevealing. Early recognition and correction of hypothermia can rapidly restore hemodynamic stability and prevent unnecessary interventions.
Hypotension with relative bradycardia in the postoperative period is uncommon and should prompt consideration of specific causes such as hypothermia, conduction disturbances, or medication effects. Hypothermia can lead to reversible cardiovascular depression by inducing bradycardia, reducing myocardial contractility, and impairing vascular tone. Environmental and physical factors must be systematically assessed in unstable postoperative patients, especially when the initial diagnostic workup is unrevealing.
Perioperative hypothermia is preventable through appropriate patient warming strategies, avoidance of prolonged exposure to cold surfaces, and vigilance against retained wet materials. Early identification and intervention can rapidly reverse hypothermia-induced instability, thereby avoiding unnecessary invasive procedures and improving patient safety.
Conclusion
Perioperative hypothermia is preventable through appropriate patient warming strategies, avoidance of prolonged exposure to cold surfaces, and vigilance against retained wet materials.
Acknowledgments: We thank the patient for consenting to publication and the medical team for their support. We also express our sincere gratitude to Dr. Zahra Hosseini for her valuable assistance in finalizing the manuscript.
Ethical Permissions: Written informed consent was obtained from the patient.
Conflicts of Interests: The authors declared no conflicts of interests.
Authors' Contribution: Alizadeh Z (First Author), Introduction Writer/Methodologist/Assistant Researcher/Discussion Writer/Statistical Analyst (30%); Zadehbagheri F (Second Author), Researcher/Discussion Writer/Statistical Analyst (25%); Jokar S (Third Author), Introduction Writer/Methodologist/Main Researcher/Discussion Writer (45%)
Funding/Support: No funding or financial support was received.
Keywords:
References
1. Tan R, Chen Y, Yang D, Long X, Ma H, Yang C. Risk factors for postoperative hypothermia in non-cardiac surgery patients: A systematic review and meta-analysis. BMC Anesthesiol. 2025;25(1):223. [Link] [DOI:10.1186/s12871-025-03089-9]
2. Wang H, Wang A, Song X, Luo J, Zhang P. Risk factors for intraoperative hypothermia during laparoscopic surgery: A systematic review and meta-analysis. PLoS One. 2025;20(7):e0328282. [Link] [DOI:10.1371/journal.pone.0328282]
3. Penjore T, Oofuvong M, Chatmongkolchart S, Kitisiripant C, Rueangchira-Urai R, Leeratiwong J. Effects of intraoperative hypothermia on patients undergoing laparoscopic surgery: A retrospective cohort study. PLoS One. 2025;20(1):e0314968. [Link] [DOI:10.1371/journal.pone.0314968]
4. Xu H, Wang Z, Guan X, Lu Y, Malone DC, Salmon JW, et al. Safety of intraoperative hypothermia for patients: Meta-analyses of randomized controlled trials and observational studies. BMC Anesthesiol. 2020;20(1):202. [Link] [DOI:10.1186/s12871-020-01065-z]
5. Yin L, Wang H, Yin X, Hu X. Impact of intraoperative hypothermia on the recovery period of anesthesia in elderly patients undergoing abdominal surgery. BMC Anesthesiol. 2024;24:124. [Link] [DOI:10.1186/s12871-024-02509-6]
6. Kim SH, Sul Y, Ye JB, Lee JY, Lee JS. Dexmedetomidine-associated hypothermia in critical trauma: A case report and literature analysis. Medicine. 2025;104(3):e41349. [Link] [DOI:10.1097/MD.0000000000041349]
7. Ilala TT, Teku Ayano G, Seife MA, Yinges Kebede M, Geleta BA, Tamrat Yilma K. Prevalence of bradycardia after induction of general anesthesia and associated factors among surgical pediatric patients. A prospective observational study. Pediatric Health Med Ther. 2023;14:419-34. [Link] [DOI:10.2147/PHMT.S429321]
8. Vanamoorthy P, Pandia MP, Bithal PK, Valiaveedan SS. Refractory hypotension due to intraoperative hypothermia during spinal instrumentation. Indian J Anaesth. 2010;54(1):56-8 [Link] [DOI:10.4103/0019-5049.60500]
9. Li L, Ye W, Li Y, Chen Y, Zeng J. Intraoperative accidental hypothermia as a probable cause of malignant ventricular arrhythmias in an elderly patient undergoing transurethral resection of prostate: A case report. Heliyon. 2023;9(8):e19006. [Link] [DOI:10.1016/j.heliyon.2023.e19006]
10. Thomson R. Hypothermia, bradycardia and hypotension in a general anesthesia case report. Crit Care Anaesth Nurs. 2018;23(3):153-6. [Link] [DOI:10.12968/coan.2018.23.3.153]
11. Rauch S, Miller C, Bräuer A, Wallner B, Bock M, Paal P. Perioperative hypothermia-a narrative review. Int J Environ Res Public Health. 2021;18(16):8749. [Link] [DOI:10.3390/ijerph18168749]
12. Hernández Alcázar EJ, Ramírez-Tapia Y, Cuevas-Hernández A, Salas-Palomino I. Perioperative hypothermia: A systematic review. REVISTA MEDICA DEL HOSPITAL GENERAL DE MEXICO. 2024;87(2). [Link] [DOI:10.24875/HGMX.23000071]
13. Wang J, Deng X. Inadvertent perioperative hypothermia: Mechanisms, risk factors, outcomes, and prevention. Anesthesiol Perioper Sci. 2023;1:24. [Link] [DOI:10.1007/s44254-023-00022-6]
14. Xu H, Xu G, Ren C, Liu L, Wei L. Effect of forced-air warming system in prevention of postoperative hypothermia in elderly patients: A prospective controlled trial. Medicine. 2019;98(22):e15895. [Link] [DOI:10.1097/MD.0000000000015895]