Volume 5, Issue 1 (2024)
J Clinic Care Skill 2024, 5(1): 49-54 |
Back to browse issues page
Article Type:
History
Received: 2023/12/18 | Accepted: 2024/03/6 | Published: 2024/03/12
Received: 2023/12/18 | Accepted: 2024/03/6 | Published: 2024/03/12
How to cite this article
NematiShahri F, Pouresmaeil O, Sharifi A, Mardani F, Mardaneh J. Genital Tuberculosis in Women; A Systematic Review. J Clinic Care Skill 2024; 5 (1) :49-54
URL: http://jccs.yums.ac.ir/article-1-229-en.html
URL: http://jccs.yums.ac.ir/article-1-229-en.html
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



Rights and permissions
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
1- Infectious Diseases Research Center, Gonabad University of Medical Sciences, Gonabad, Iran
2- Microbiology Laboratory, Allameh Bohlool Hospital, Gonabad University of Medical Sciences, Gonabad, Iran
3- “Department of Microbiology, School of Medicine” and “Infectious Diseases Research Centre”, Gonabad University of Medical Sciences, Gonabad, Iran
2- Microbiology Laboratory, Allameh Bohlool Hospital, Gonabad University of Medical Sciences, Gonabad, Iran
3- “Department of Microbiology, School of Medicine” and “Infectious Diseases Research Centre”, Gonabad University of Medical Sciences, Gonabad, Iran
Full-Text (HTML) (2483 Views)
Introduction
Tuberculosis (TB), caused by bacteria belonging to the Mycobacterium tuberculosis complex, is one of the most common causes of death from infectious diseases worldwide [1]. The WHO reports that in 2019, an estimated 10 million people fell ill with tuberculosis (TB) worldwide. Tuberculosis after the Second World War was nearly eradicated in developed countries due to the spread of vaccination, early diagnosis, appropriate treatment, and improvements in life standards. However, in recent years, it has risen again due to increased migration and immunodeficiency diseases such as HIV, and it remains a major health problem in underdeveloped countries [2]. The disease is usually classified as pulmonary or extrapulmonary. Pulmonary tuberculosis (PTB) constitutes the more common clinical presentation of TB, and extrapulmonary involvement includes about a third of the cases [1]. The most common sites involved in extrapulmonary tuberculosis are the lymph nodes, pleura, bones, meninges, and urogenital tract. Genitourinary tuberculosis accounts for 15% of all extrapulmonary cases and can include various organs such as the ovaries, fallopian tubes, uterus, cervix, and vulva [3]. Female genital tuberculosis (FGTB) is generally caused by the reactivation of organisms from the systemic dissemination of Mycobacterium tuberculosis during the initial infection. The distribution occurs usually through hematogenous or lymphatic routes. Genital tuberculosis is rare, and its true prevalence is not specified because many cases remain unknown. Genital tuberculosis is mostly asymptomatic; However, genital tuberculosis can be clinically associated with different signs and symptoms such as infertility, amenorrhea, ascites, abdominal pain, and postmenopausal bleeding. Patients with FGTB receive similar medical therapy as patients with pulmonary TB, and excellent FGTB treatment rates have been reported. In the review of the literature, no comprehensive study was found addressing the systematic review of genital tuberculosis in females. This systematic review aimed to describe the epidemiology, clinical presentation, diagnosis, and treatment of FGTB during 2000-2021 and provide a new perspective on FGTB worldwide.
Information and Methods
This systematic review was conducted on the global literature on tuberculosis in the female reproductive system and vulva between 2000 and 2021. Various databases, including PubMed, Scopus, Embase, Web of Science, and Google Scholar, were utilized to gather the relevant studies. The retrieval process focused on English keywords like “female genital tuberculosis”, “vulva tuberculosis”, “tuberculosis”, “genital system” as well as Persian keywords. A similar approach was taken to identify related Persian articles in Iranian databases specific to Iran, such as Irandoc and Magiran. All types of studies (original, case reports, etc.) related to the theme of the present research were examined, but case report studies were the primary source of suitable articles. This review includes case report studies featuring female patients diagnosed with vulva or genital tuberculosis. Both English and Persian articles were considered for potential inclusion. The exclusion criteria were the unavailability of full-text articles, systematic reviews, narrative-only conference abstracts, multiple reports of the same data, and non-scientific diagnostic methods. 568 references in Persian and English were obtained from various research databases. After the elimination of duplicate entries, 72 references were retained and underwent abstract analysis conducted independently by two reviewers. Out of these, 52 references were considered to meet eligibility criteria. 23 references were excluded after the full-text review, and 29 studies satisfied the eligibility criteria and were consequently included in the analysis (Figure 1).
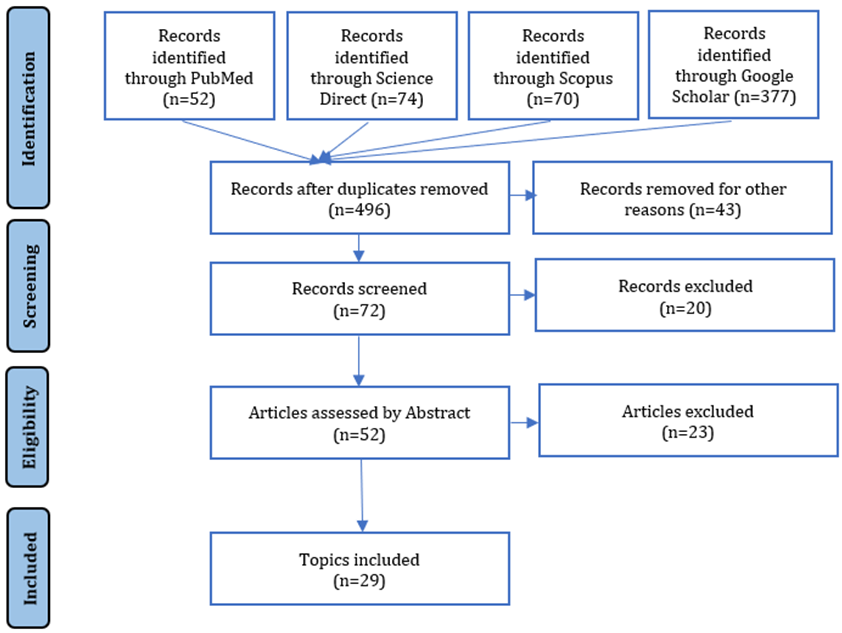
Figure 1. Included and excluded data flowchart
The critical appraisal checklist provided by the Joanna Briggs Institute (JBI) was employed to evaluate the overall quality of studies. This checklist has 8 parts and addresses various sections of the reports. Two reviewers independently assessed the validity of the studies.
Findings
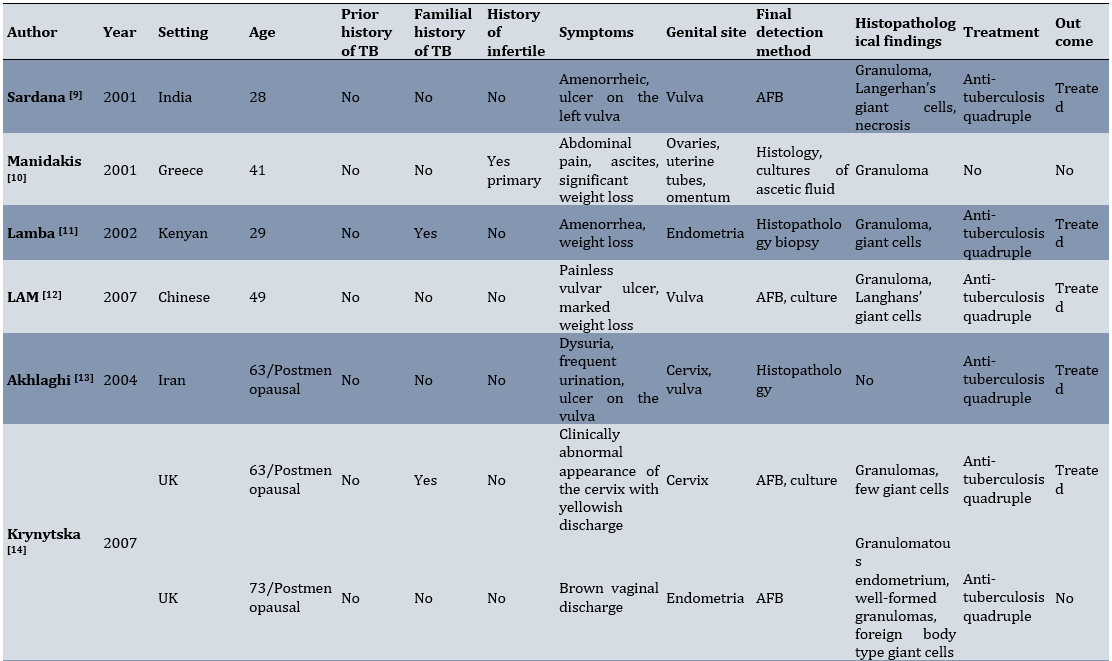
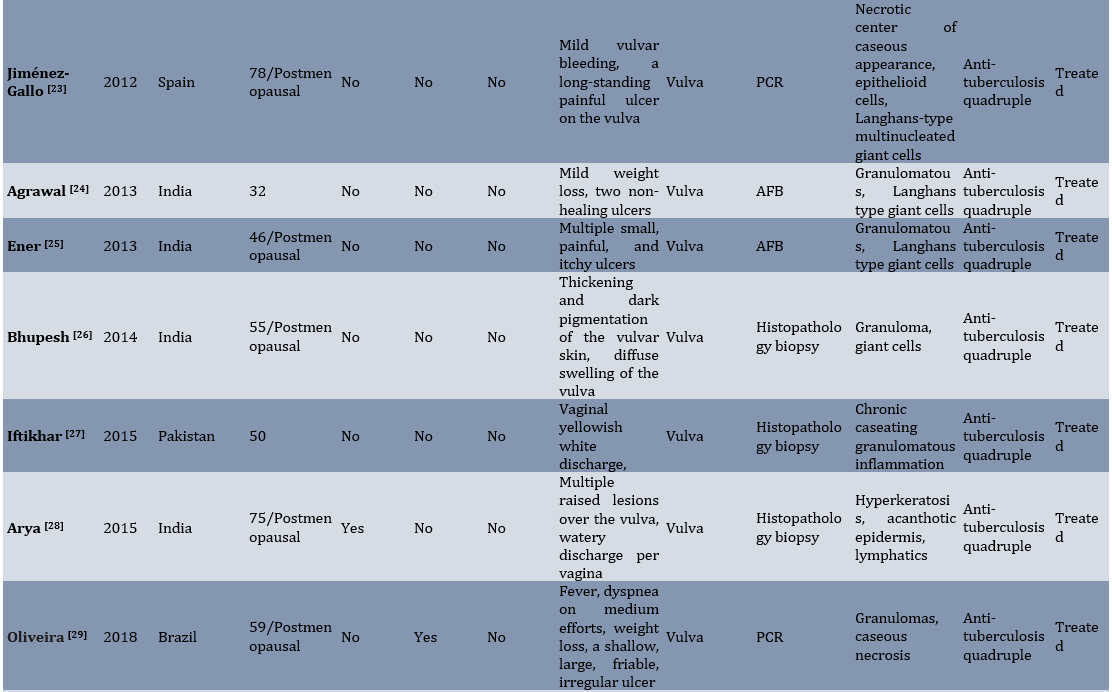
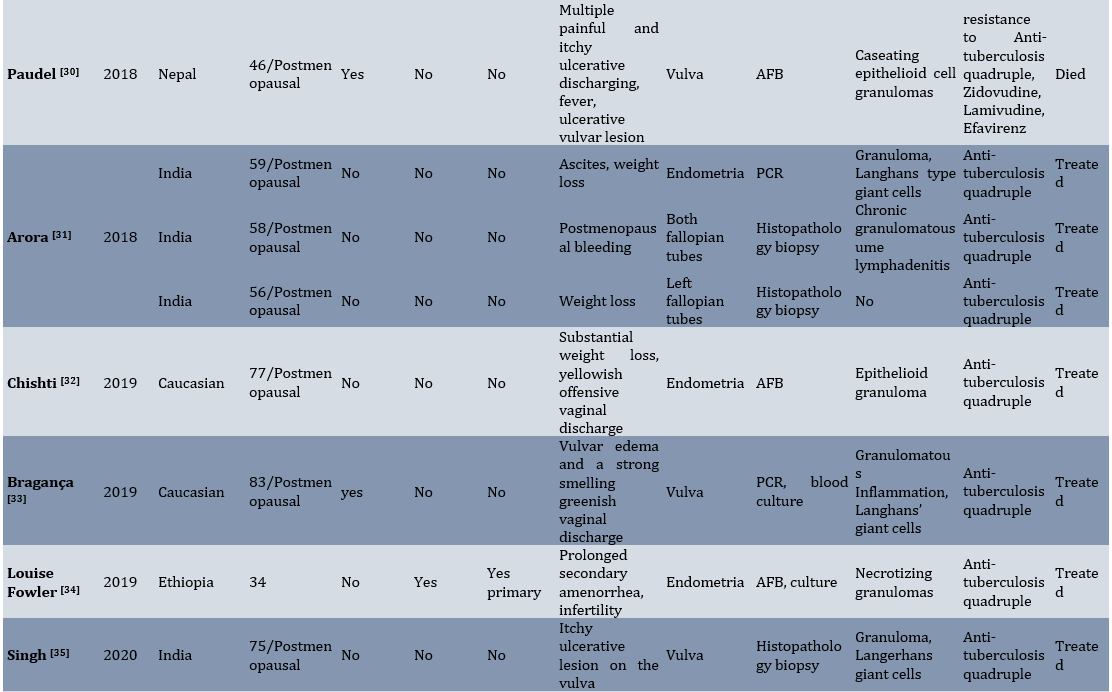
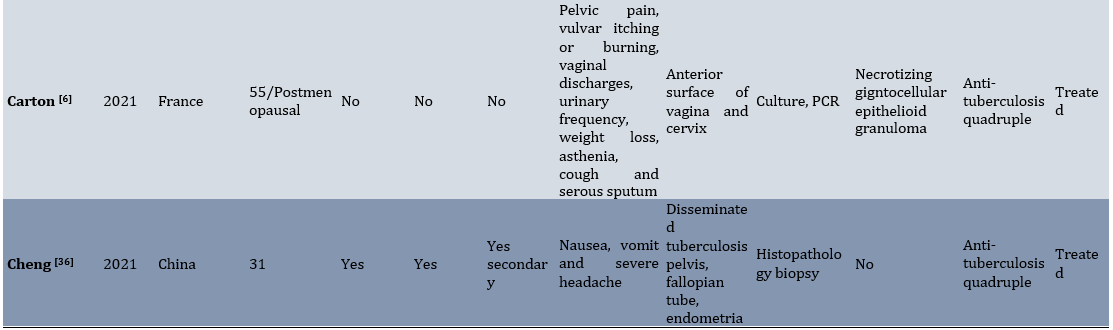
During the twenty-one-year observational period (2000-2021), data about 32 patients with FGTB from 14 countries and regions was collected (Table 1).
Table 1. Data extracted from articles

The distribution of ages among the cases ranged from 14 to 83 years, with a median age of 52.5 years. 59.4% of the study population were postmenopausal women, while 40.6% of patients were their reproductive age. Five women (15.6%) had a history of pulmonary TB, and five other women had a familial history of TB. The geographical distribution of the FGT patients indicated that most were from India (12, 37.5%). It is revealed that the incidence of genital tuberculosis is high in countries with low socio-economic levels and poor people. The distribution of genital tuberculosis according to the involved organs was as follows: 16 cases (50%) of the vulva, 5 cases (15.6%) of the endometrium, 3 cases (9.3%) of the cervix, and 3 cases (9.3%) fallopian tubes. There were also multiple organ involvements in 5 cases (15.6%). Amongst four positive cases (12.5%) with infertility, three cases suffered from primary infertility, while one case had secondary infertility. Fertility data were not available in three single patients. Among the patients with infertility complaints, one case had endometrial TB, one case was diagnosed as cervical TB, and two cases had disseminated tuberculosis. The clinical features of genital tuberculosis are generally non‑specific. Weight loss (31.25%) and vaginal discharge (31.25%) were the most common symptoms reported by the study participants. Other symptoms, such as amenorrhea, ascites, abdominal pain, postmenopausal bleeding, and fever, were less prevalent among patients. In all the patients with vulvar tuberculosis, the most common clinical complaint was the appearance of an ulcer on the outer area of the vulva. These ulcers had different clinical features, such as itch and pain. The main histologic finding in female genital TB was the presence of epithelioid cell granulomas that were observed in 81.25% of patients. Langhans-type multinucleated giant cells were present in 46.87% of the cases. Acid-fast bacilli (AFB) in tissue sections were detected in 46.87% of cases after Ziehl-Neelsen (ZN) staining. Seven patients (21.87%) had positive PCR results. 29 (90.6%) patients received the standard antibiotic therapy (combination of rifampicin, isoniazid, ethambutol, and pyrazinamide), resulting in a favorable treatment response for all individuals. Information regarding the treatment and outcomes of two patients remained undisclosed. Notably, treatment resistance was documented in only one case. An alternative regimen, including Zidovudine, Lamivudine, and Efavirenz, was used for a particular female patient who unfortunately succumbed to the illness. It is crucial to highlight that the patient was confirmed to be HIV positive.
Discussion
The present study was conducted to perform a systematic review of studies that aims to describe the epidemiology, clinical presentation, diagnosis, and treatment of FGTB between 2000-2021 and to provide a fresh perspective on FGTB. The prevalence of female genital tuberculosis is often underestimated due to its low occurrence in developed countries, challenging and delayed diagnosis, and various nonspecific signs and symptoms. Consequently, the incidence of this illness in the communities cannot be accurately determined [4]. Female genital tuberculosis is more prevalent in underdeveloped and developing countries, particularly in India. It is indicated that the occurrence of TB is higher in economically disadvantaged countries with low socio-economic status, poverty, and residence. These factors can be considered as epidemiological factors related with the diagnosis of female genital tuberculosis. However, the examination of a small number of patients from developed countries indicates that genital TB in these countries has not been entirely eliminated and should be considered. Female genital TB can affect females of all age groups. The age range of the cases spanned from 14 to 83 with a median age of 52.5 years. Genital tuberculosis can be categorized based on the site of infection and semiology; Upper genital tuberculosis affects the fallopian tubes, endometrium, ovaries, and uterus. Lower genital tuberculosis, on the other hand, affect the cervix, vagina, and vulva [5]. Upper genital tuberculosis can manifest with very diverse clinical presentations and lead to a variety of symptoms including amenorrhea, ascites, chronic abdominal pain, pelvic pain, weight loss, fever, and serious complication such as infertility [6]. Lower genital tuberculosis, especially in the vulva, typically manifest as ulcers on the outer surfaces of the vulva. This study showed that the unpleasant appearance of vulvar tuberculosis in patients varies from ulcerative lesions, lymphedema, or grossly hypertrophic lesions to discharging sinuses with different clinical features such as pain and itch. The incidence of vulva tuberculosis was found to be 68% in postmenopausal women. There is no explanation behind the prevalence of vulvar tuberculosis in this age group. Studies have indicated that atrophic endometrium is an unfavorable environment for the growth of Mycobacterium in women who have gone through menopause [7]. Therefore, tuberculosis is more likely to induce infections in the lower genital area in this specific group of women. Diagnosis of vulvar tuberculosis is difficult. The clinical appearance of vulva tubercular ulcers can be quite variable and lead to potential misdiagnosis as a sexually transmitted disease such as syphilis, chancroid, or carcinoma [8]. Weight loss was the predominant symptom identified among all the patients. Although weight loss is a nonspecific indication of tuberculosis and can also be present in many other diseases. However, due to the high prevalence of this symptom among patients, it can raise suspicion of tuberculosis.
The limitation of this study was the absence of complete textual content for some articles within the databases.
Conclusion
Most patients experience prolonged vulva ulcers. Occasionally, due to misdiagnosis, the patient inadvertently received various antibiotics. The typical lesions in female genital TB are epithelioid cell granulomas which may or may not be accompanied by Langerhans giant cells. Following an accurate diagnosis of genital tuberculosis, the majority of the patients exhibited a favorable response to treatment, resulting in the disappearance of illness symptoms.
Acknowledgments: We thank Gonabad University of Medical Sciences for supporting this study.
Ethical Permissions: None declared by the authors.
Conflicts of Interests: The authors had no conflict of interest.
Tuberculosis (TB), caused by bacteria belonging to the Mycobacterium tuberculosis complex, is one of the most common causes of death from infectious diseases worldwide [1]. The WHO reports that in 2019, an estimated 10 million people fell ill with tuberculosis (TB) worldwide. Tuberculosis after the Second World War was nearly eradicated in developed countries due to the spread of vaccination, early diagnosis, appropriate treatment, and improvements in life standards. However, in recent years, it has risen again due to increased migration and immunodeficiency diseases such as HIV, and it remains a major health problem in underdeveloped countries [2]. The disease is usually classified as pulmonary or extrapulmonary. Pulmonary tuberculosis (PTB) constitutes the more common clinical presentation of TB, and extrapulmonary involvement includes about a third of the cases [1]. The most common sites involved in extrapulmonary tuberculosis are the lymph nodes, pleura, bones, meninges, and urogenital tract. Genitourinary tuberculosis accounts for 15% of all extrapulmonary cases and can include various organs such as the ovaries, fallopian tubes, uterus, cervix, and vulva [3]. Female genital tuberculosis (FGTB) is generally caused by the reactivation of organisms from the systemic dissemination of Mycobacterium tuberculosis during the initial infection. The distribution occurs usually through hematogenous or lymphatic routes. Genital tuberculosis is rare, and its true prevalence is not specified because many cases remain unknown. Genital tuberculosis is mostly asymptomatic; However, genital tuberculosis can be clinically associated with different signs and symptoms such as infertility, amenorrhea, ascites, abdominal pain, and postmenopausal bleeding. Patients with FGTB receive similar medical therapy as patients with pulmonary TB, and excellent FGTB treatment rates have been reported. In the review of the literature, no comprehensive study was found addressing the systematic review of genital tuberculosis in females. This systematic review aimed to describe the epidemiology, clinical presentation, diagnosis, and treatment of FGTB during 2000-2021 and provide a new perspective on FGTB worldwide.
Information and Methods
This systematic review was conducted on the global literature on tuberculosis in the female reproductive system and vulva between 2000 and 2021. Various databases, including PubMed, Scopus, Embase, Web of Science, and Google Scholar, were utilized to gather the relevant studies. The retrieval process focused on English keywords like “female genital tuberculosis”, “vulva tuberculosis”, “tuberculosis”, “genital system” as well as Persian keywords. A similar approach was taken to identify related Persian articles in Iranian databases specific to Iran, such as Irandoc and Magiran. All types of studies (original, case reports, etc.) related to the theme of the present research were examined, but case report studies were the primary source of suitable articles. This review includes case report studies featuring female patients diagnosed with vulva or genital tuberculosis. Both English and Persian articles were considered for potential inclusion. The exclusion criteria were the unavailability of full-text articles, systematic reviews, narrative-only conference abstracts, multiple reports of the same data, and non-scientific diagnostic methods. 568 references in Persian and English were obtained from various research databases. After the elimination of duplicate entries, 72 references were retained and underwent abstract analysis conducted independently by two reviewers. Out of these, 52 references were considered to meet eligibility criteria. 23 references were excluded after the full-text review, and 29 studies satisfied the eligibility criteria and were consequently included in the analysis (Figure 1).
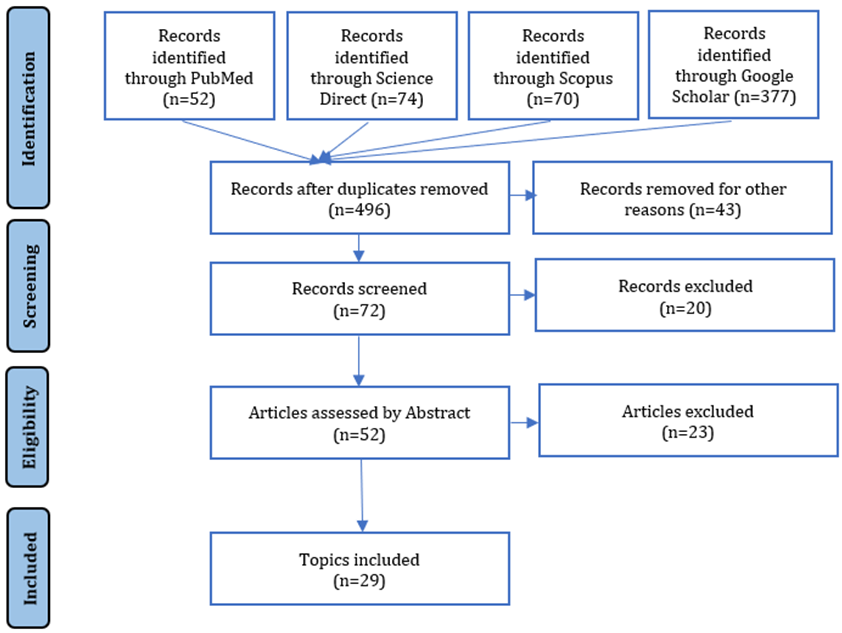
Figure 1. Included and excluded data flowchart
The critical appraisal checklist provided by the Joanna Briggs Institute (JBI) was employed to evaluate the overall quality of studies. This checklist has 8 parts and addresses various sections of the reports. Two reviewers independently assessed the validity of the studies.
Findings
During the twenty-one-year observational period (2000-2021), data about 32 patients with FGTB from 14 countries and regions was collected (Table 1).
Table 1. Data extracted from articles
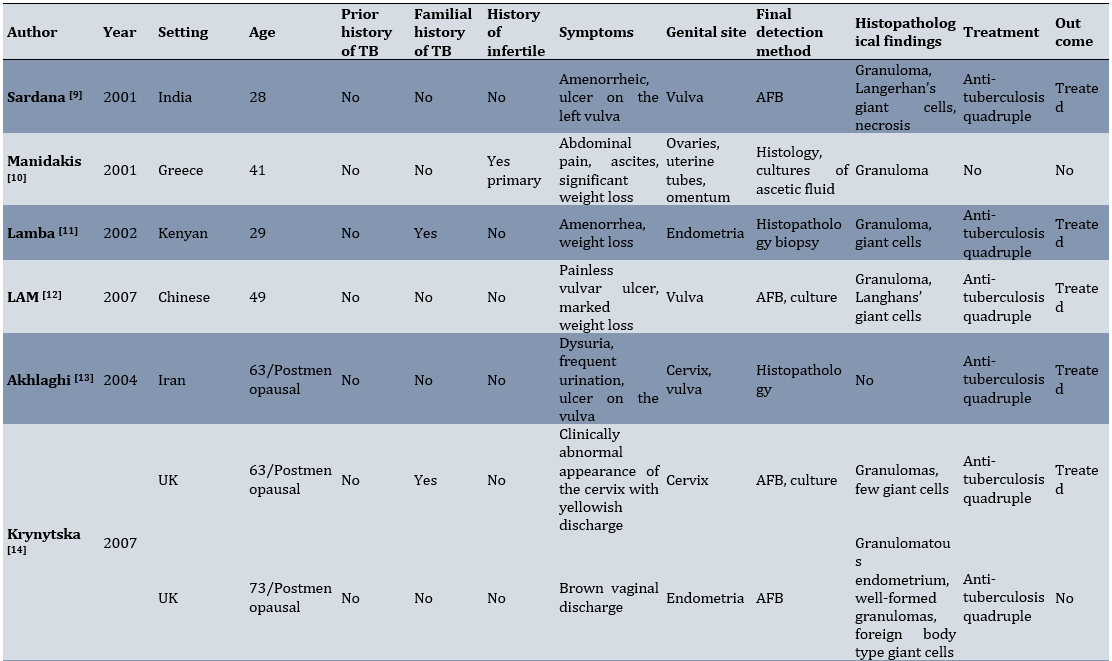

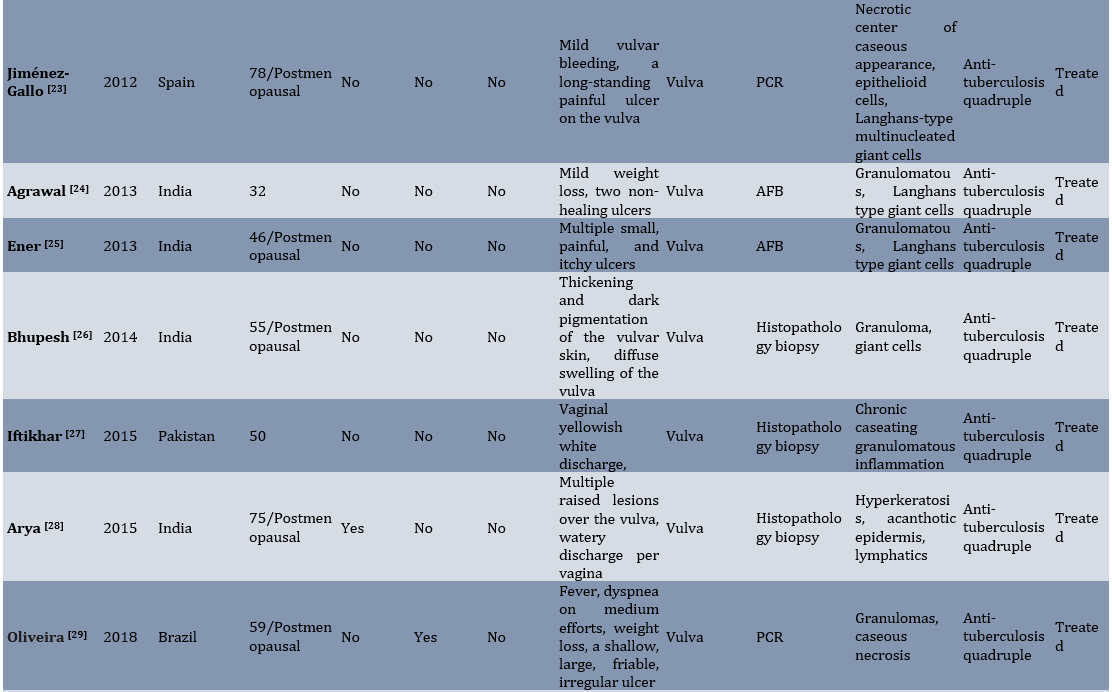
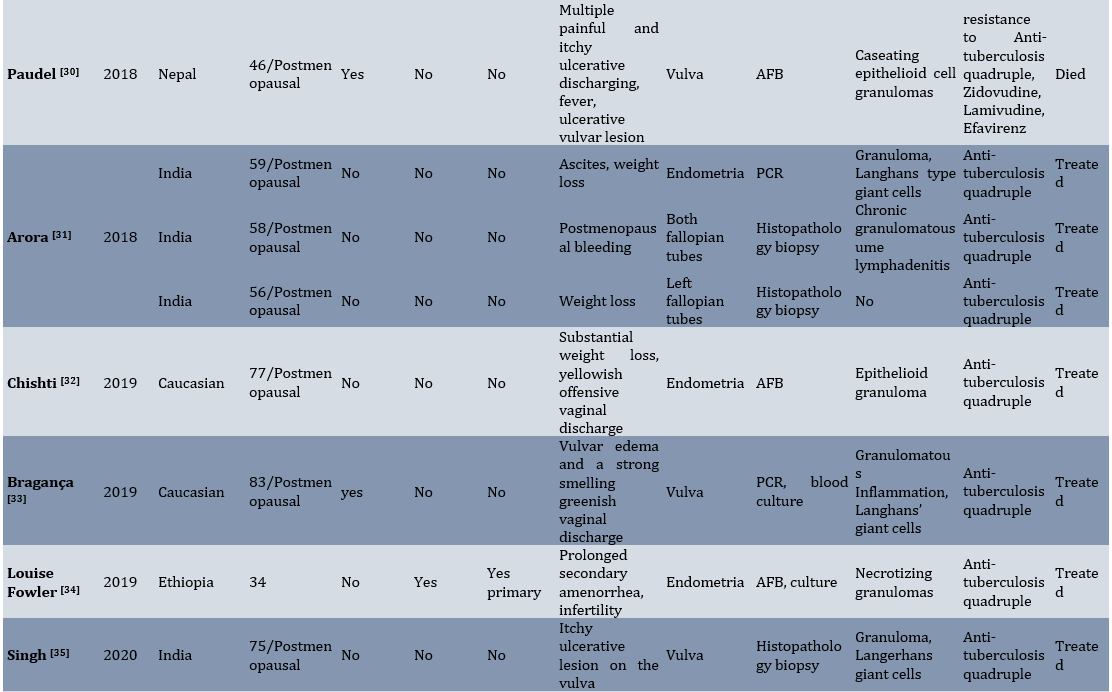
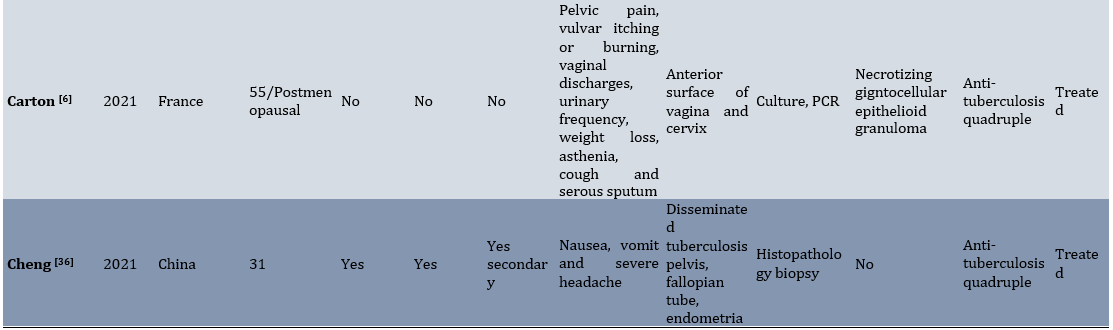
The distribution of ages among the cases ranged from 14 to 83 years, with a median age of 52.5 years. 59.4% of the study population were postmenopausal women, while 40.6% of patients were their reproductive age. Five women (15.6%) had a history of pulmonary TB, and five other women had a familial history of TB. The geographical distribution of the FGT patients indicated that most were from India (12, 37.5%). It is revealed that the incidence of genital tuberculosis is high in countries with low socio-economic levels and poor people. The distribution of genital tuberculosis according to the involved organs was as follows: 16 cases (50%) of the vulva, 5 cases (15.6%) of the endometrium, 3 cases (9.3%) of the cervix, and 3 cases (9.3%) fallopian tubes. There were also multiple organ involvements in 5 cases (15.6%). Amongst four positive cases (12.5%) with infertility, three cases suffered from primary infertility, while one case had secondary infertility. Fertility data were not available in three single patients. Among the patients with infertility complaints, one case had endometrial TB, one case was diagnosed as cervical TB, and two cases had disseminated tuberculosis. The clinical features of genital tuberculosis are generally non‑specific. Weight loss (31.25%) and vaginal discharge (31.25%) were the most common symptoms reported by the study participants. Other symptoms, such as amenorrhea, ascites, abdominal pain, postmenopausal bleeding, and fever, were less prevalent among patients. In all the patients with vulvar tuberculosis, the most common clinical complaint was the appearance of an ulcer on the outer area of the vulva. These ulcers had different clinical features, such as itch and pain. The main histologic finding in female genital TB was the presence of epithelioid cell granulomas that were observed in 81.25% of patients. Langhans-type multinucleated giant cells were present in 46.87% of the cases. Acid-fast bacilli (AFB) in tissue sections were detected in 46.87% of cases after Ziehl-Neelsen (ZN) staining. Seven patients (21.87%) had positive PCR results. 29 (90.6%) patients received the standard antibiotic therapy (combination of rifampicin, isoniazid, ethambutol, and pyrazinamide), resulting in a favorable treatment response for all individuals. Information regarding the treatment and outcomes of two patients remained undisclosed. Notably, treatment resistance was documented in only one case. An alternative regimen, including Zidovudine, Lamivudine, and Efavirenz, was used for a particular female patient who unfortunately succumbed to the illness. It is crucial to highlight that the patient was confirmed to be HIV positive.
Discussion
The present study was conducted to perform a systematic review of studies that aims to describe the epidemiology, clinical presentation, diagnosis, and treatment of FGTB between 2000-2021 and to provide a fresh perspective on FGTB. The prevalence of female genital tuberculosis is often underestimated due to its low occurrence in developed countries, challenging and delayed diagnosis, and various nonspecific signs and symptoms. Consequently, the incidence of this illness in the communities cannot be accurately determined [4]. Female genital tuberculosis is more prevalent in underdeveloped and developing countries, particularly in India. It is indicated that the occurrence of TB is higher in economically disadvantaged countries with low socio-economic status, poverty, and residence. These factors can be considered as epidemiological factors related with the diagnosis of female genital tuberculosis. However, the examination of a small number of patients from developed countries indicates that genital TB in these countries has not been entirely eliminated and should be considered. Female genital TB can affect females of all age groups. The age range of the cases spanned from 14 to 83 with a median age of 52.5 years. Genital tuberculosis can be categorized based on the site of infection and semiology; Upper genital tuberculosis affects the fallopian tubes, endometrium, ovaries, and uterus. Lower genital tuberculosis, on the other hand, affect the cervix, vagina, and vulva [5]. Upper genital tuberculosis can manifest with very diverse clinical presentations and lead to a variety of symptoms including amenorrhea, ascites, chronic abdominal pain, pelvic pain, weight loss, fever, and serious complication such as infertility [6]. Lower genital tuberculosis, especially in the vulva, typically manifest as ulcers on the outer surfaces of the vulva. This study showed that the unpleasant appearance of vulvar tuberculosis in patients varies from ulcerative lesions, lymphedema, or grossly hypertrophic lesions to discharging sinuses with different clinical features such as pain and itch. The incidence of vulva tuberculosis was found to be 68% in postmenopausal women. There is no explanation behind the prevalence of vulvar tuberculosis in this age group. Studies have indicated that atrophic endometrium is an unfavorable environment for the growth of Mycobacterium in women who have gone through menopause [7]. Therefore, tuberculosis is more likely to induce infections in the lower genital area in this specific group of women. Diagnosis of vulvar tuberculosis is difficult. The clinical appearance of vulva tubercular ulcers can be quite variable and lead to potential misdiagnosis as a sexually transmitted disease such as syphilis, chancroid, or carcinoma [8]. Weight loss was the predominant symptom identified among all the patients. Although weight loss is a nonspecific indication of tuberculosis and can also be present in many other diseases. However, due to the high prevalence of this symptom among patients, it can raise suspicion of tuberculosis.
The limitation of this study was the absence of complete textual content for some articles within the databases.
Conclusion
Most patients experience prolonged vulva ulcers. Occasionally, due to misdiagnosis, the patient inadvertently received various antibiotics. The typical lesions in female genital TB are epithelioid cell granulomas which may or may not be accompanied by Langerhans giant cells. Following an accurate diagnosis of genital tuberculosis, the majority of the patients exhibited a favorable response to treatment, resulting in the disappearance of illness symptoms.
Acknowledgments: We thank Gonabad University of Medical Sciences for supporting this study.
Ethical Permissions: None declared by the authors.
Conflicts of Interests: The authors had no conflict of interest.
Authors’ Contribution: NematiShahri F (First Author), Introduction Writer (20%); Pouresmaeil O (Second Author), Introduction Writer/Assistant Researcher/Discussion Writer (30%); Sharifi A (Third Author), Discussion Writer/Statistical Analyst (10%); Mardani F (Fourth Author), Assistant Researcher/Discussion Writer(10%); Mardaneh J (Fifth Author), Methodologist/Main Researcher/Discussion Writer (30%)
Funding/Support: This work was financially supported by Gonabad University of Medical Sciences, Gonabad, Iran.
Keywords:
References
1. Muneer A, Macrae B, Krishnamoorthy S, Zumla A. Urogenital tuberculosis-epidemiology, pathogenesis and clinical features. Nat Rev Urol. 2019;16(10):573-98. [Link] [DOI:10.1038/s41585-019-0228-9]
2. Hsu CT, Yang LC, Hsu ML, Chen WH, Lin UN. The coexistence of carcinoma and tuberculosis in the uterine cervix: Report of 2 cases. Asia‐Ocean J Obstet Gynaecol. 1985;11(3):363-9. [Link] [DOI:10.1111/j.1447-0756.1985.tb00756.x]
3. Lee JY. Diagnosis and treatment of extrapulmonary tuberculosis. Tuberc Respir Dis. 2015;78(2):47-55. [Link] [DOI:10.4046/trd.2015.78.2.47]
4. Gatongi DK, Gitau G, Kay V, Ngwenya S, Lafong C, Hasan A. Female genital tuberculosis. Obstet Gynaecol. 2005;7(2):75-9. [Link] [DOI:10.1576/toag.7.2.075.27000]
5. Chowdhury NN. Overview of tuberculosis of the female genital tract. J Indian Med Assoc. 1996;94(9):345-61. [Link]
6. Carton I, Balès D, Bargain A, Lemoine PLP. Vaginal tuberculosis as differential diagnosis of cancer: A case report. J Gynecol Obstet Hum Reprod. 2021;50(6):101873. [Link] [DOI:10.1016/j.jogoh.2020.101873]
7. Güngördük K, Ulker V, Sahbaz A, Ark C, Tekırdag AI. Postmenopausal tuberculosis endometritis. Infect Dis Obstet Gynecol. 2007;2007:27028. [Link] [DOI:10.1155/2007/27028]
8. Kaur T, Dhawan S, Aggarwal A, Bansal S. Vulval tuberculosis. J Obstet Gynaecol India. 2012;62(4):450-1. [Link] [DOI:10.1007/s13224-012-0131-2]
9. Sardana K, Koranne RV, Sharma RC, Mahajan S. Tuberculosis of the vulva masquerading as a sexually transmitted disease. J Dermatol. 2001;28(9):505-7. [Link] [DOI:10.1111/j.1346-8138.2001.tb00020.x]
10. Manidakis LG, Angelakis E, Sifakis S, Stefanaki P, Kalogeraki A, Manidaki A, et al. Genital tuberculosis can present as disseminated ovarian carcinoma with ascites and raised Ca-125: A case report. Gynecol Obstet Invest. 2001;51(4):277-9. [Link] [DOI:10.1159/000058065]
11. Lamba H, Byrne M, Goldin R, Jenkins C. Tuberculosis of the cervix: Case presentation and a review of the literature. Sex Transm Infect. 2002;78(1):62-3. [Link] [DOI:10.1136/sti.78.1.62]
12. Lam SK, Chan KS, Chin R. A rare case of vulvar tuberculosis. Hong Kong J Gynaecol Obstet Midwifery. 2007;7(1):56. [Link]
13. Akhlaghi F, Farazmand T. A rare case report of tuberculosis of the cervix and vulva in Zeinab Hospital in Mashhad. Razi J Med Sci. 2004;11(40):181-4. [Persian] [Link]
14. Krynytska I, Firket C. Genital tuberculosis in postmenopausal patients. J Obstet Gynaecol. 2007;27(4):444-5. [Link] [DOI:10.1080/01443610701359837]
15. Paprikar M, Biswas M, Bhattacharyav S, Sodhi B, Mukhopadhyay I. Tuberculosis of cervix. Med J Armed Forces India. 2008;64(3):297-8. [Link] [DOI:10.1016/S0377-1237(08)80129-3]
16. Agrawal S, Madan M, Leekha N, Raghunandan C. A rare case of cervical tuberculosis simulating carcinoma cervix: A case report. Cases J. 2009;2:161. [Link] [DOI:10.1186/1757-1626-2-161]
17. Gupta R, Dey P, Jain V, Gupta N. Cervical tuberculosis detection in Papanicolaou‐stained smear: Case report with review of literature. Diagn Cytopathol. 2009;37(8):592-5. [Link] [DOI:10.1002/dc.21082]
18. Ilmer M, Bergauer F, Friese K, Mylonas I. Genital tuberculosis as the cause of tuboovarian abscess in an immunosuppressed patient. Infect Dis Obstet Gynecol. 2009;2009:745060. [Link] [DOI:10.1155/2009/745060]
19. Buppasiri P, Temtanakitpaisan T, Somboonporn W. Tuberculosis at vulva and vagina. J Med Assoc Thai. 2010;93(5):613-5. [Link]
20. Keshavarzi F, Fakheri T, Nankali A. Vulvar tuberculosis in a virgin girl: A rare case report. Int J Collab Res Intern Med Public Health. 2012;4(5):825-8. [Link]
21. Shen HP, Chang WC, Hsieh CH, Yang TC, Hung YC. Vulvar tuberculosis. Taiwan J Obstet Gynecol. 2011;50(1):106-8. [Link] [DOI:10.1016/j.tjog.2009.10.002]
22. Kitisupornpun S, Mahanupab P, Intapibool S. A case report; Tuberculosis of the vulva. Chiang Mai Med J. 2011;50(4):123-8. [Link]
23. Jiménez-Gallo D, Navas-García N, Albarrán-Planelles C, Guerrero-Sánchez F. Periorificial cutaneous tuberculosis of the vulva. ACTAS Dermo-Sifiliográficas. 2012;103(10):929-30. [Link] [DOI:10.1016/j.adengl.2011.12.004]
24. Agrawal DR. Primary tuberculosis vulva-A case report. Natl J Integr Res Med. 2013;4(1):142-3. [Link]
25. Krishnendu M, Shwetank M, Malay B, Dilip P, Moumita M, Partha PM. Primary vulval tuberculosis presenting as multiple vulval ulcers: A rare case report. UroToday Int J. 2013;6(3):39. [Link]
26. Goyal BK, Pradhan S, Jose T, Duggal BS, Sengupta P. Woody vulva: An unusual presentation of vulvar tuberculosis. J Obstet Gynaecol India. 2014; 64(Suppl 1):85-7. [Link] [DOI:10.1007/s13224-012-0325-7]
27. Iftikhar N, Kiyani S. A rare case of vulval tuberculosis. Isra Med J. 2015;7(2):111-3. [Link]
28. Arya S, Nyati A, Bunkar M, Takhar RP, Mirdha S. Cutaneous lymphangiectasia of the vulva secondary to pulmonary tuberculosis: A case report. Int J Res Dermatol. 2015;1(1):14-16. [Link] [DOI:10.18203/issn.2455-4529.IntJResDermatol20160351]
29. Oliveira M, Vita-Campos C, Jeunon T. Vulvar tuberculosis cutis orificialis concomitant to pulmonary tuberculosis: A case report. Am J Dermatopathol. 2018;40(12):908-11. [Link] [DOI:10.1097/DAD.0000000000001182]
30. Paudel V, Chudal D, Pokhrel DB. Tuberculosis and HIV co-infection; The deadly duos in vulva. Indian J Tuberc. 2018;65(4):277-9. [Link] [DOI:10.1016/j.ijtb.2018.05.016]
31. Arora A, Sadath SA. Genital tuberculosis in postmenopausal women with variable clinical presentations: A report of 3 cases. Case Rep Womens Health. 2018;18:e00059. [Link] [DOI:10.1016/j.crwh.2018.e00059]
32. Chishti U, Elorbany S, Akhtar M, Williams J, Heenan S, Barton DP. Genital tuberculosis in a post-menopausal Caucasian woman: A case report. J Obstet Gynaecol. 2019;39(2):284-5. [Link] [DOI:10.1080/01443615.2018.1468741]
33. Bragança C, Gonçalves I, Guerreiro L, Janeiro M. Vulvar tuberculosis-A rare manifestation of the disease. Revista Brasileira de Ginecologia e Obstetrícia. 2019;41(9):575-8. [Link] [DOI:10.1055/s-0039-1695020]
34. Fowler ML, Mahalingaiah S. Case report of pelvic tuberculosis resulting in Asherman's syndrome and infertility. Fertil Res Pract. 2019;5:8. [Link] [DOI:10.1186/s40738-019-0061-0]
35. Singh V, Singh G, Sinha RJ, Babu S. Vulvar tuberculosis. BMJ Case Rep. 2020;13(2):e232880. [Link] [DOI:10.1136/bcr-2019-232880]
36. Cheng M, Yuan T, Liu Y. A woman with disseminated tuberculosis experienced preterm delivery, fallopian tube pregnancy, and delivered successfully following in vitro fertilization: A case report. BMC Pregnancy Childbirth. 2021;21:27. [Link] [DOI:10.1186/s12884-020-03487-6]










