Volume 5, Issue 1 (2024)
J Clinic Care Skill 2024, 5(1): 1-4 |
Back to browse issues page
Article Type:
History
Received: 2023/11/8 | Accepted: 2024/01/11 | Published: 2024/02/21
Received: 2023/11/8 | Accepted: 2024/01/11 | Published: 2024/02/21
How to cite this article
Ganjali H, Attaran H, Hedjazi A, Chavoshi H. Lethal Intracranial Injury as a Complication of Septorhinoplasty; A Case Report. J Clinic Care Skill 2024; 5 (1) :1-4
URL: http://jccs.yums.ac.ir/article-1-219-en.html
URL: http://jccs.yums.ac.ir/article-1-219-en.html
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



Rights and permissions
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
1- Legal Medicine Research Center, Tehran, Iran
Full-Text (HTML) (844 Views)
Introduction
Nasal septoplasty is one of the most commonly performed procedures in otorhinolaryngology and plastic surgery. The primary indication for this functional surgery is usually septal deviation resulting in significant and symptomatic nasal airway obstruction [1]. There are several complications accompanying septoplasty. The most common complications of septoplasty are deformities, infections, and perforations [2]. Rare complications include cavernous sinus thrombosis, meningitis, pneumocephalus, subarachnoid hemorrhage, periorbital emphysema, toxic shock syndrome, brain abscess, and cerebrospinal fluid (CSF) leak [3]. Although rare, intracranial complications of septorhinoplasty are life-threatening, and there are few case reports on fatal intracranial complications [4].
Najari et al. reported a case of death following septoplasty. In this case, cerebral edema, an intraparenchymal hematoma in the left frontal lobe, and pneumocephalus on the surface of both frontal lobes in addition to a saccular aneurysm of the left ophthalmic artery led to patient death [4].
Tawadros et al. presented another case of someone who died after septoplasty due to extensive subarachnoid and intraventricular hemorrhage and hydrocephalus [5]. Moreover, Peyvandi & Roozbahany described a case who underwent septoplasty to correct the septal deviation. The day after surgery, the patient’s level of consciousness decreased due to hemorrhage in all brain ventricles, especially in the right lateral ventricle, causing hydrocephalous and hernia and pressure effect on the midline structure with a slight shift to the left. There was also pneumocephalus in the right temporal horn. The patient was in a vegetative state and died after approximately 1 month of stay in the intensive care unit [6].
Herein, we present a case of a healthy 47-year-old woman who underwent septorhinoplasty, then had a decreased level of consciousness, and finally died due to subarachnoid and intraventricular hemorrhage caused by a bone fragment isolated from the fractured sphenoid sinus.
Patient and Methods
An otherwise healthy 47-year-old woman with severely deviated nasal septum, which caused spurs of bone and deformity and decreased airway space behind the soft palate, was planned for septorhinoplasty by a board-certified plastic surgeon. The patient was admitted to a day surgery unit for elective surgery. The pre-operative assessment was performed using a CT scan (Figure 1).

Figure 1. Pre-operation CT scan of Paranasal Sinuses
Findings
During the operation, the patient was under anesthesia for 4 hours and 40 minutes. According to the anesthesiologist's report, the patient lost 1500-1700cc of blood during the procedure, which was controlled using a tampon. The surgeon did not mention the source of the bleeding in the operation note. The anesthesiologist administered 1gr of transaminase, intramuscular vitamin K, and 3 liters of normal saline, and there was about 1 liter of urine output after urinary bladder catheterization.
The patient’s blood sugar was 244mg/dl immediately after the operation. Her respiratory state was not good enough for extubation and did not improve after two hours. The patient received naloxone. However, she still had miotic and non-reactive pupils. Thereafter, 250mg of aminophylline was administered, and blood sugar was checked again, and it was 457 mg. Therefore, the patient received 10U of subcutaneous regular insulin. Regarding a decreased Hb of 7.1, a packed cell transfusion was done, and she was transferred to the intensive care unit.
Despite the discontinuation of sedatives, the patient remained unconscious. A brain spiral computed tomography scan was performed, which revealed a fracture with displacement of bone fragments of the posterior wall of the sphenoid sinus on both sides and the dorsum sellae and posterior clinoid, as well as the nasal bone (Figure 2). Intraventricular hemorrhage was evident in the ventricular system, and hyperdensity of basal cisterns suggesting subarachnoid hemorrhage (SAH) was observed. The final diagnosis was considered brain stem ischemia, intraventricular hemorrhage (IVH), and SAH due to traumatic injury to paranasal sinuses. The patient was transferred to the neurosurgery unit and underwent ventriculostomy, but interventions were not effective, and she died after seven days.
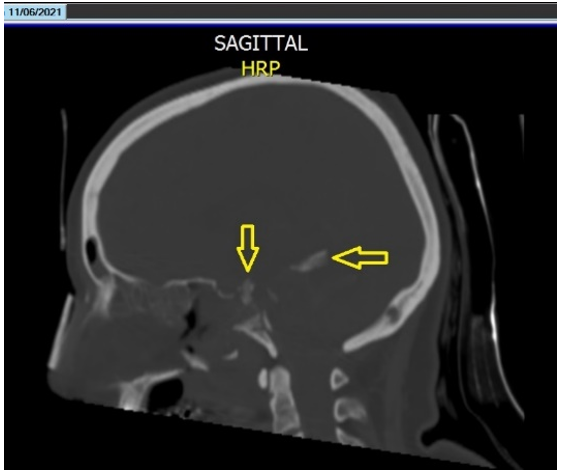
Figure 2. Penetration of bone fragments into the brain tissue
At autopsy, cerebral edema and SAH in the right frontal area and cerebellum were evident. Examination of the skull base showed a fracture in front of the Sella turcica (Figure 3) and penetration of bone fragments into the brain tissue. Also, hematoma was seen in the brainstem. The cause of death was declared cerebral hemorrhage and its complications following skull base fracture during surgery.
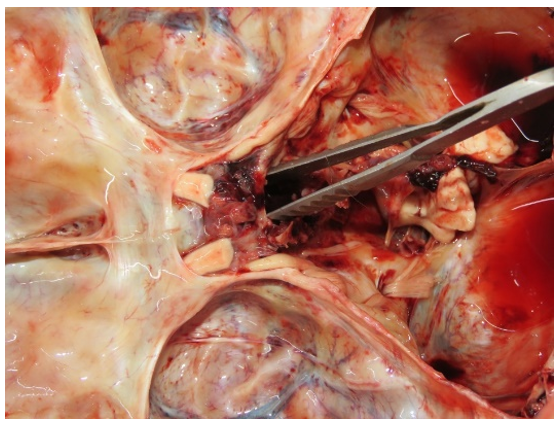
Figure 3. Skull base fracture in front of the sella turcica.
Discussion
As previously mentioned, skull base injury following septoplasty is a rare complication, and few such cases have been reported. In this case, the patient died due to SAH and IVH following sinus bone fracture and penetration of bone fragments into the brain tissue.
Accordingly, the septoplasty surgeon must comprehensively understand the relevant anatomy, with a specific appreciation for high-risk areas. Although a study by Bateman and colleagues has shown that no single surgical maneuver could be identified or associated with an increased risk for septoplasty complications, the need for meticulous surgical technique remains evident [7].
In 2014, Günaydın et al. reported a case in which the posterior part of the sphenoid sinus was broken, and a bone fragment was observed in the right compartment of the sphenoid. In this case, a brain CT scan revealed pneumocephalus without any cerebral hemorrhage. The patient underwent an operation and recovered [8]. In the present report, the broken bone fragments penetrated the brain tissue and caused SAH and IVH leading to death.
According to the results of a 2009 study conducted by Bloom et al., complications after septoplasty are rare and can be limited by experience, meticulous surgical technique, and comprehensive preoperative planning.
In this report, the sphenoid sinus was broken, which should not normally be manipulated in this type of surgery. This might be due to the surgeon's inexperience, lack of accurate knowledge of the area's anatomy, or even job fatigue.
Regarding the results achieved by Gray et al., traumatic skull base injuries can be divided into iatrogenic (e.g., Surgical) and accidental. The most common cause of iatrogenic skull base injury is endoscopic sinus surgery. Intraoperative injury most commonly occurs at the ethmoid roof and the lateral lamella of the cribriform plate [9]. So, it might lead to a cerebrospinal fluid (CSF) leak due to the opening of the dural space to the nasopharynx.
The reported rate of CSF leak as the most common complication of endoscopic sinus surgery is less than 1%. However, in this case, the sphenoid sinus was damaged, and the patient did not recover from anesthesia, so there was no time for CSF rhinorrhea to be detected. Moreover, in this case, the used technique was open surgery.
As a preventive measure, a study by Ali has demonstrated that a CT scan of the nose and paranasal sinuses plays a critical role in the preoperative assessment of patients admitted for endoscopic sinus surgeries for chronic rhinosinusitis. The asymmetry of the ethmoid fovea, olfactory fossa, anatomical variations of the lateral lamella, and course of the anterior ethmoid artery is essential in ESS as it may become prone to life-threatening adverse effects such as hemorrhage, CSF leak, and even intracranial complications [10].
Research Limitations: The treating surgeon's omission of details about the events during the surgery in the surgical procedure report has made it difficult to accurately determine the exact mechanism of the injuries.
Conclusion
It seems that surgeon experience in septoplasty surgery is crucial, and meticulous attention to anatomical landmarks is of paramount importance to prevent a disastrous outcome that may lead to patient death and surgeon conviction.
Acknowledgment: The authors would like to thank the forensic medical autopsy department of Mashhad Legal Medicine Organization for granting access to the autopsy report and images.
Ethical Permissions: The case report was authorized by the ethics committee of the Legal Medicine Organization.
Conflicts of Interests: The authors declare no conflicts of interest in this case report.
Authors’ Contribution: Ganjali H (First Author), Main Researcher/Introduction Writer (25%); Attaran H (Second Author), Main Researcher/Methodologist (25%); Hedjazi A (Third Author), Main Researcher/Data Analyst (25%); Chavoshi H (Fourth Author), Main Researcher/Discussion Writer (25%)
Funding/Support: The authors received no financial support for the research, authorship, and/or publication of this article.
Nasal septoplasty is one of the most commonly performed procedures in otorhinolaryngology and plastic surgery. The primary indication for this functional surgery is usually septal deviation resulting in significant and symptomatic nasal airway obstruction [1]. There are several complications accompanying septoplasty. The most common complications of septoplasty are deformities, infections, and perforations [2]. Rare complications include cavernous sinus thrombosis, meningitis, pneumocephalus, subarachnoid hemorrhage, periorbital emphysema, toxic shock syndrome, brain abscess, and cerebrospinal fluid (CSF) leak [3]. Although rare, intracranial complications of septorhinoplasty are life-threatening, and there are few case reports on fatal intracranial complications [4].
Najari et al. reported a case of death following septoplasty. In this case, cerebral edema, an intraparenchymal hematoma in the left frontal lobe, and pneumocephalus on the surface of both frontal lobes in addition to a saccular aneurysm of the left ophthalmic artery led to patient death [4].
Tawadros et al. presented another case of someone who died after septoplasty due to extensive subarachnoid and intraventricular hemorrhage and hydrocephalus [5]. Moreover, Peyvandi & Roozbahany described a case who underwent septoplasty to correct the septal deviation. The day after surgery, the patient’s level of consciousness decreased due to hemorrhage in all brain ventricles, especially in the right lateral ventricle, causing hydrocephalous and hernia and pressure effect on the midline structure with a slight shift to the left. There was also pneumocephalus in the right temporal horn. The patient was in a vegetative state and died after approximately 1 month of stay in the intensive care unit [6].
Herein, we present a case of a healthy 47-year-old woman who underwent septorhinoplasty, then had a decreased level of consciousness, and finally died due to subarachnoid and intraventricular hemorrhage caused by a bone fragment isolated from the fractured sphenoid sinus.
Patient and Methods
An otherwise healthy 47-year-old woman with severely deviated nasal septum, which caused spurs of bone and deformity and decreased airway space behind the soft palate, was planned for septorhinoplasty by a board-certified plastic surgeon. The patient was admitted to a day surgery unit for elective surgery. The pre-operative assessment was performed using a CT scan (Figure 1).

Figure 1. Pre-operation CT scan of Paranasal Sinuses
Findings
During the operation, the patient was under anesthesia for 4 hours and 40 minutes. According to the anesthesiologist's report, the patient lost 1500-1700cc of blood during the procedure, which was controlled using a tampon. The surgeon did not mention the source of the bleeding in the operation note. The anesthesiologist administered 1gr of transaminase, intramuscular vitamin K, and 3 liters of normal saline, and there was about 1 liter of urine output after urinary bladder catheterization.
The patient’s blood sugar was 244mg/dl immediately after the operation. Her respiratory state was not good enough for extubation and did not improve after two hours. The patient received naloxone. However, she still had miotic and non-reactive pupils. Thereafter, 250mg of aminophylline was administered, and blood sugar was checked again, and it was 457 mg. Therefore, the patient received 10U of subcutaneous regular insulin. Regarding a decreased Hb of 7.1, a packed cell transfusion was done, and she was transferred to the intensive care unit.
Despite the discontinuation of sedatives, the patient remained unconscious. A brain spiral computed tomography scan was performed, which revealed a fracture with displacement of bone fragments of the posterior wall of the sphenoid sinus on both sides and the dorsum sellae and posterior clinoid, as well as the nasal bone (Figure 2). Intraventricular hemorrhage was evident in the ventricular system, and hyperdensity of basal cisterns suggesting subarachnoid hemorrhage (SAH) was observed. The final diagnosis was considered brain stem ischemia, intraventricular hemorrhage (IVH), and SAH due to traumatic injury to paranasal sinuses. The patient was transferred to the neurosurgery unit and underwent ventriculostomy, but interventions were not effective, and she died after seven days.
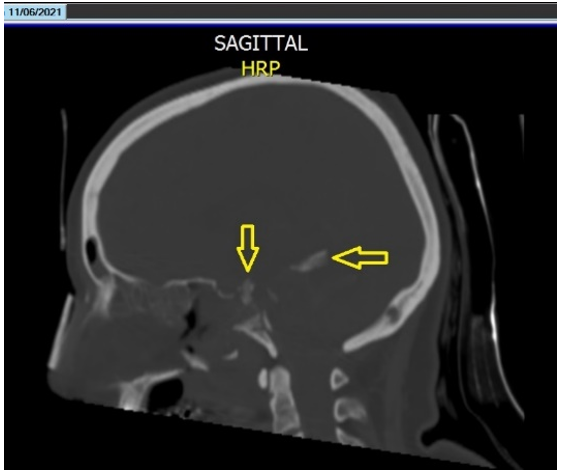
Figure 2. Penetration of bone fragments into the brain tissue
At autopsy, cerebral edema and SAH in the right frontal area and cerebellum were evident. Examination of the skull base showed a fracture in front of the Sella turcica (Figure 3) and penetration of bone fragments into the brain tissue. Also, hematoma was seen in the brainstem. The cause of death was declared cerebral hemorrhage and its complications following skull base fracture during surgery.
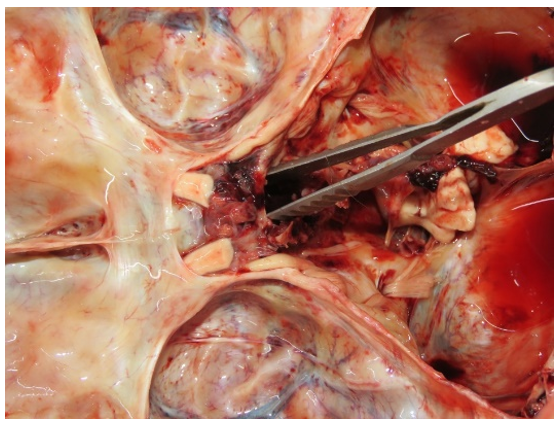
Figure 3. Skull base fracture in front of the sella turcica.
Discussion
As previously mentioned, skull base injury following septoplasty is a rare complication, and few such cases have been reported. In this case, the patient died due to SAH and IVH following sinus bone fracture and penetration of bone fragments into the brain tissue.
Accordingly, the septoplasty surgeon must comprehensively understand the relevant anatomy, with a specific appreciation for high-risk areas. Although a study by Bateman and colleagues has shown that no single surgical maneuver could be identified or associated with an increased risk for septoplasty complications, the need for meticulous surgical technique remains evident [7].
In 2014, Günaydın et al. reported a case in which the posterior part of the sphenoid sinus was broken, and a bone fragment was observed in the right compartment of the sphenoid. In this case, a brain CT scan revealed pneumocephalus without any cerebral hemorrhage. The patient underwent an operation and recovered [8]. In the present report, the broken bone fragments penetrated the brain tissue and caused SAH and IVH leading to death.
According to the results of a 2009 study conducted by Bloom et al., complications after septoplasty are rare and can be limited by experience, meticulous surgical technique, and comprehensive preoperative planning.
In this report, the sphenoid sinus was broken, which should not normally be manipulated in this type of surgery. This might be due to the surgeon's inexperience, lack of accurate knowledge of the area's anatomy, or even job fatigue.
Regarding the results achieved by Gray et al., traumatic skull base injuries can be divided into iatrogenic (e.g., Surgical) and accidental. The most common cause of iatrogenic skull base injury is endoscopic sinus surgery. Intraoperative injury most commonly occurs at the ethmoid roof and the lateral lamella of the cribriform plate [9]. So, it might lead to a cerebrospinal fluid (CSF) leak due to the opening of the dural space to the nasopharynx.
The reported rate of CSF leak as the most common complication of endoscopic sinus surgery is less than 1%. However, in this case, the sphenoid sinus was damaged, and the patient did not recover from anesthesia, so there was no time for CSF rhinorrhea to be detected. Moreover, in this case, the used technique was open surgery.
As a preventive measure, a study by Ali has demonstrated that a CT scan of the nose and paranasal sinuses plays a critical role in the preoperative assessment of patients admitted for endoscopic sinus surgeries for chronic rhinosinusitis. The asymmetry of the ethmoid fovea, olfactory fossa, anatomical variations of the lateral lamella, and course of the anterior ethmoid artery is essential in ESS as it may become prone to life-threatening adverse effects such as hemorrhage, CSF leak, and even intracranial complications [10].
Research Limitations: The treating surgeon's omission of details about the events during the surgery in the surgical procedure report has made it difficult to accurately determine the exact mechanism of the injuries.
Conclusion
It seems that surgeon experience in septoplasty surgery is crucial, and meticulous attention to anatomical landmarks is of paramount importance to prevent a disastrous outcome that may lead to patient death and surgeon conviction.
Acknowledgment: The authors would like to thank the forensic medical autopsy department of Mashhad Legal Medicine Organization for granting access to the autopsy report and images.
Ethical Permissions: The case report was authorized by the ethics committee of the Legal Medicine Organization.
Conflicts of Interests: The authors declare no conflicts of interest in this case report.
Authors’ Contribution: Ganjali H (First Author), Main Researcher/Introduction Writer (25%); Attaran H (Second Author), Main Researcher/Methodologist (25%); Hedjazi A (Third Author), Main Researcher/Data Analyst (25%); Chavoshi H (Fourth Author), Main Researcher/Discussion Writer (25%)
Funding/Support: The authors received no financial support for the research, authorship, and/or publication of this article.
Keywords:
References
1. Watters C, Brar S, Yapa S. Septoplasty. Treasure Island, FL: StatPearls; 2021. [Link]
2. Alotaibi AD. The common complications after septoplasty and septorhinoplasty: A report in a series of 127 cases. Int J Otolaryngol Head Neck Surg. 2017;6(6):71-8. [Link] [DOI:10.4236/ijohns.2017.66010]
3. Ahmed Youssef SA, Ahmed Aly Ibrahim, Mulvihill Daniel, Hisham M. Abdelfattah, Haitham Morsi. Traumatic cerebrospinal fluid leakage following septorhinoplasty. Arch Plast Surg 2018;45(4):379-83. [Link] [DOI:10.5999/aps.2017.00913]
4. Najari F, Ghadipasha M, Alimohammadi A, Kayal IB, Saravani K. A case report of intracranial complication following. Iran Red Crescent Med J. 2017;19(10):e13905. [Link] [DOI:10.5812/ircmj.13905]
5. Tawadros AM, Prahlow JA. Death related to nasal surgery. Am J Forensic Med Pathol. 2008;29(3):260-4. [Link] [DOI:10.1097/PAF.0b013e3181832432]
6. Peyvandi A, Roozbahany NA. Skull base injury leading to death after conventional septoplasty. Am J Forensic Med Pathol. 2013;34(1):5-6. [Link] [DOI:10.1097/PAF.0b013e3182518e31]
7. Bateman N, Woolford T. Informed consent for septal surgery: the evidence-base. J Laryngol Otol. 2003;117(3):186-9. [Link] [DOI:10.1258/002221503321192476]
8. Günaydın RÖ, Özer S, Süslü N, Yücel ÖT. Sphenoid sinus injury leading pneumocephalus as a complication of conventional septoplasty. Turk Arch Otolaryngol. 2014;52:70-3. [Link] [DOI:10.5152/tao.2014.143]
9. Gray ST, Wu AW. Pathophysiology of iatrogenic and traumatic skull base injury. Adv Otorhinolaryngol. 2013;74:12-23. [Link] [DOI:10.1159/000342264]
10. Ali A, Kurien M, Shyamkumar NK, Selvaraj. Anterior skull base: High risk areas in endoscopic sinus surgery in chronic rhinosinusitis: A computed tomographic analysis. Indian J Otolaryngol Head Neck Surg. 2005;57(1):5-8. [Link] [DOI:10.1007/BF02907616]









