Received: 2024/01/10 | Accepted: 2024/03/4 | Published: 2024/03/12
URL: http://jccs.yums.ac.ir/article-1-233-en.html
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
2- Department of Sport Injuries and Corrective Exercises, Astara Branch, Islamic Azad University, Astara, Iran
3- Research Center for Health Sciences, Hamadan University of Medical Sciences, Hamadan, Iran
Overhead sports require substantial kinetic energy transference through the shoulder at rapid speeds through large ranges of motion with high precision [1]. Scapular dyskinesis (SD) refers to the altered position and motion of the scapula [2]. SD has a higher prevalence (61%) in overhead athletes compared with non-overhead athletes (33%) [3]. SD is present in 67% to 100% of athletes with shoulder injuries. However, it is also present in many asymptomatic individuals [4]. SD has been associated with shoulder pain, specifically shoulder impingement syndrome (SIS), rotator cuff tendinopathy, and multidirectional impairments [2, 5]. It is reported that athletes with SD have a 43% greater risk of developing shoulder pain than those without SD [6]. In overhead athletes, the scapular joints experience increased stress during throwing as the ‘‘funnel’’ or bridge transfers power from the lower extremities and trunk to the arm [2, 7, 8]. Alterations in this transfer of power lead to increased stress on the glenohumeral and scapular-thoracic joints, thus increasing the theoretical risk of injury [7, 9]. Therefore, scapula position in both static and dynamic states is an important risk factor for shoulder injuries in overhead sports [10]. On the other hand, in overhead athletes, the high repetition of the movement pattern may cause adaptive changes in the structure and musculoskeletal function of the shoulder girdle [11]. This situation may gradually affect the shoulder joint's stabilizing mechanisms, mainly rotator cuff muscles [12]. It can cause weakness in the glenohumeral external rotator (ER) muscles and muscle imbalance in the rotator cuff [13, 14]. Rotator cuff weakness and imbalance may impair motor control, resulting in superior translation of the humeral head and further mechanical abrasion of the structures of the subacromial space [6]. It is accepted that a low concentric external/internal strength ratio (ER:IR) may lead to excessive humeral head anterior displacement and increase the loading on the biceps long head tendon. Furthermore, the eccentric strength of the external rotator is not only important for acceleration in the cocking phase of throwing and the entering phase of swimming but also for deceleration and control in the follow-through and recovery phase [15]. It is also believed that eccentric strength must be as strong as concentric internal rotation to maintain normal shoulder function [10, 16]. SD and ER muscle weakness are a causative factor of shoulder injuries in overhead athletes [2, 10, 16-18]. ER weakness [19], lower ER:IR, and SD may be risk factors identifying elite handball players at higher risk of injury and requiring preventive intervention [16, 18, 20-22].
Exercise therapy is frequently recommended to overhead athletes with shoulder injuries who are diagnosed with SD and scapular muscle imbalance to correct the faulty scapular position and improve function [23, 24]. Therefore, many authors have emphasized the need to correct SD and increase ER muscle strength and endurance during rehabilitation programs [2, 13].
Moura et al. also found that amateur athletes with subacromial pain syndrome associated with SD responded well to a rehabilitation program [13]. The training program of Tang et al. also emphasized shoulder stabilization exercises and improved shoulder function and SD in patients with shoulder arthritis and SD [25]. Based on a systematic review of the literature that was conducted to evaluate the role of exercise in the treatment of rotator cuff impingement and synthesis of a standard evidence-based rehabilitation protocol. Although many of the articles had methodological concerns, the data showed that exercise had a statistically and clinically significant effect on reducing pain and improving function but not on range of motion or strength [26]. According to Yuksel & Yesilyaprak, Scapular stabilization exercises added to the shoulder mobilization, stretching, and strengthening exercises are effective in improving SD, reducing pain, increasing muscle strength and shoulder function in patients with Subacromial pain syndrome (SAPS) accompanied by SD [27]. However, Hotta et al. found that the inclusion of the isolated scapular stabilization exercises, emphasizing retraction and depression of the scapula, to a progressive general periscapular strengthening protocol did not add benefits to shoulder pain and disability, muscle strength, and ROM in patients with SAPS [28].
Some exercise programs emphasized scapular control, correction of muscular imbalance, and sensory-motor training [13] or shoulder stabilization exercises [28]. Some others focus on shoulder mobilization exercises, Scapular stabilization, stretching [29], and strengthening exercises [27]. As mentioned, there is no consensus on whether the exercises effectively correct scapular position and reduce rotator cuff muscle imbalance. Also, in most studies, exercises have been presented for individuals with shoulder pain and clinical disorders such as impingement syndrome. There is a lack of studies investigating the factors mentioned in asymptomatic overhead athletes. Therefore, this study aimed to investigate the effect of an exercise program on SD and the strength of glenohumeral rotator cuff muscles in overhead athletes.
Materials and Methods
Design
This study, which used the quasi-experimental method with a control group and a pre- and post-test plan, was conducted from 2021 to 2022 in Hamadan City, Iran. The population of this study is female handball players (club-level, 18–25 years old) with SD in Hamadan city, Iran. A total of 221 handball players were identified and evaluated by an experienced physiotherapist, and according to the inclusion and exclusion criteria, 62 subjects with SD were selected using the convenience sampling method. A block randomization method with a block size of four was used to randomize participants. For this purpose, four sheets of paper were prepared. The letter I (under treatment with exercise program) was written on two sheets, and the letter C (control group) was written on the other two sheets. The sheets were mixed and randomly drawn out one at a time for each participant without replacement until all four sheets were drawn. This method was repeated until all participants were randomized (each group 31). The study's inclusion criteria consisted of the female gender, having at least three years of regular sports experience in handball, and the presence of SD. The exclusion criteria consisted of pain in the shoulder girdle and neck in the normal and practice conditions; history of fracture or dislocation in each shoulder girdle bone; complete rupture of shoulder girdle muscles; positive Neer impingement test or Hawkins impingement test; and history of surgery in the shoulder girdle.
Measurement and Data Gathering
Scapular Dyskinesis
To assess SD, the scapula lateral sliding test provided by Kibler was used [10]. In this test, the distance of the lower angle of each scapula from the adjacent vertebra was measured with a tape measure in three positions of 0.45 and 90 degrees of arm abduction. Each measurement was repeated thrice on both hands, and their average was calculated. If there is a difference of 1.5cm or more between the two shoulders, the test is positive. Kibler has reported the intra-group reliability of this test from 0.84 to 0.88 and its out-group reliability from 0.77 to 0.85 in different angles [30].
Internal and external rotation strength of the shoulder
A handheld dynamometer (Lafayette; USA) was used to measure the isometric IR and ER strength. The subject was supine by adopting 90 degrees of shoulder abduction and 90 degrees of elbow flexion (while the forearm was perpendicular to the ground). An assistant stabilized the shoulder, and then the subject maximally resisted against the dynamometer, placing 2 cm below the styloid process in the ventral face of the wrist (for IR) and dorsal face (for ER). The maximum isometric force of the individual was recorded in kilograms on the digital screen of the device [31]. Each test was repeated three times with a one-minute break between them, and then their average was recorded. At the same time, the measurements were performed on the dominant hand of the subjects.
In this study, the intervention is a modified exercise protocol from Moura et al. The intervention group received the exercise protocol from Moura et al. [13]. The program used included the modified exercise protocol of Moura et al. (Table 1) [13], which was repeated by the experimental group three sessions per week with moderate intensity for eight weeks. The exercise program consisted of three phases, the first phase focusing on scapular control and increasing the range of motion, the second phase on increasing the strength of the scapular muscles and sensorimotor exercises, and the third phase on advanced sensorimotor exercises. All exercises were performed in 3 sets with 15 repetitions. The rest between each set was gradually reduced until the end of the period. Data Were measured within a week before and after the intervention. Also, the control group subjects were advised to continue their usual exercise routine. The control group received only routine exercises.
In this protocol, we attempted to minimize biases by randomizing subjects, blinding the assessor (who did not know the subjects' allocation). However, the researcher responsible for the intervention was not blinded due to the characteristics of the intervention.
Table 1. Selected corrective exercise protocol

Statistical Analysis
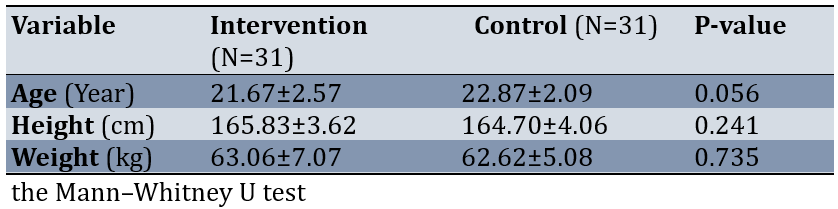
The data were analyzed using SPSS 23 software. The normality of variables was investigated using the Shapiro-Wilk test. Mann-Whitney U test was used to compare the demographic variables between the two groups. In addition, the Mann-Whitney U test was used to compare the mean strength of IR, ER, and SD, as divided by the time intervals before and after the intervention between the two groups. All statistical analyses were performed at p<0.05 significant levels.
Findings
62 individuals participated and remained until the end of the study. There were no statistically significant differences between intervention and control groups in mean age (p=0.056), height (p=0.241), and weight (p=0.735; Table 2).
Table 2. Demographic Characteristics of the Intervention and Control Group
The strength of ER and ER:IR increased after exercises in the intervention group (p<0.001). Also, SD after exercises has decreased significantly (p=0.013; Table 3).
Table 3. Comparison of the mean score of strength of the ER and SD between the two groups by Mann–Whitney U test

Discussion
This study aimed to investigate the effect of exercise programs on SD, ER strength, and rotator cuff balance (ER:IR strength) in female handball players. SD is characterized by reduced scapular upward rotation, increased scapular internal rotation and anterior tilt, and reduced range of motion. These positions create scapular protraction, and decrease demonstrated rotator cuff strength [32]. The results of the study showed that the exercise program caused a significant decrease in the SD and an increase in ER and ER:IR strength in handball players.
Moura et al. by presenting an exercise program similar to the present study, found that SD decreased, and ER strength and ER/IR ratio increased in athletes with subacromial pain syndrome [13]. These results agree with the findings of our study. In the present study, the exercise program included three phases. The focus of the first phase was on controlling the scapula and increasing the range of motion, the second phase was on increasing the strength of the scapular muscles and sensorimotor exercises, and the third phase was on advanced sensorimotor exercises [13]. The study of Hotta et al. revealed Motor control and muscular strengthening training lasting for 8 weeks influenced the resting position (SD) and scapular movement pattern of subjects with shoulder impingement syndrome [34]. Various authors have suggested that neuromuscular control and strengthening of the periscapular muscles are important in treating SD in shoulder injuries [13]. Scapular-focused treatment includes a variety of interventions directed at the soft tissues functionally related to the scapula, such as periscapular strengthening, stretching, mobilization [33], stability/stabilization, and motor control of the scapula [33-35]. A study by Baskurt et al. on patients with subacromial impingement syndrome showed the efficacy of proprioceptive neuromuscular facilitation exercises for scapular muscles [35].
Activation sequencing patterns and strength of the muscles that stabilize the scapula are altered in patients with SD [2]. Increased upper trapezius activity, imbalance of upper trapezius/lower trapezius activation, and decreased serratus anterior activity have been reported in these patients [32]. The serratus anterior is most important as an external rotator of the scapula, and the lower trapezius stabilizes the acquired scapular position [1]. Scapular stabilization protocols should focus on re-educating these muscles to act as dynamic scapula stabilizers first via the implementation of short lever, kinetic chain assisted exercises, then progress to long lever movements [32]; this is an issue that has been done in all three phases of the exercise program of the current study, by including exercises such as push-up plus, punch exercise, prone Cobra, prone horizontal abduction. It seems that Scapular stabilization exercises added to the shoulder mobilization, stretching, and strengthening are effective in improving SD, reducing pain, and increasing muscle strength and shoulder function in patients with Subacromial pain syndrome accompanied by SD [25, 27]. Hotta et al. mentioned that including the isolated scapular stabilization exercises in a progressive periscapular strengthening, protocol did not benefit disability, muscle strength, and range of motion in patients with subacromial pain syndrome. The difference in the results of the mentioned study can be related to the type of selected exercises. Also, the samples were not athletes [28]. There are some inconsistencies in the results regarding the efficacy of therapeutic exercises on SD and the strength of ER. Methodologic heterogeneity could be a reason for the conflicting results.
Another study found an increase in ER and ER:IR strength (rotator cuff balance) after the exercise program. The scapular position, which provides a stable base of support for the rotator cuff muscles, is retraction and external rotation. Conversely, when the scapula is protracted in SD, the maximal rotator cuff strength decreases because of reduced force-generating capabilities for the internal and external rotators [36]. This situation creates conditions for rotator cuff muscle imbalance [2]. Merolla et al. reported the weakness of supraspinatus and infraspinatus due to SD, explaining that the first step in the rehabilitation program is strengthening the periscapular muscles [36]. Therefore, the inclusion of all the exercises from the present study, such as push-up plus, punch, prone horizontal abduction, and prone cobra, which strengthen the periscapular muscles and improve SD [13], is also considered the first stage of rotator cuff muscle imbalance rehabilitation [36]. Rotator cuff emphasis in rehabilitation should be after scapular control is achieved. A logical progression of exercises focused on strengthening the lower trapezius and serratus anterior while minimizing upper trapezius activation has been described in the literature [32]. Stabilization exercises, which include stretching and strengthening exercises with emphasis on the position and movement of the scapula, allow the scapula to act as a basis for muscle activity, as well as the role of the link in the proximal to the distal transfer of energy for the appropriate shoulder positioning [37].
In the present study, performing rotator cuff strengthening exercises, including external rotation with and without the riband, in the second and third phases of the exercise program is associated with an increase in ER and ER:IR strength [13, 36]. Moura et al. obtained similar results. They found that ER and ER:IR strength increased after performing an exercise program similar to our study [13].
One of the strengths of the study was its preventive approach to injury. Also, to eliminate some nuisance variables, such as the difference in the movement pattern of different sports, the samples were selected from only one sport (handball). The limitation of the present study was the low number of studies that used non-pathological athletes. The majority of studies were conducted on athletes with subacromial pain syndrome. Also, other variables related to SD, such as glenohumeral rotation range of motion and electromyography of periscapular muscles, were not measured. However, future studies with standard, reliable, and valid measurement techniques with more participants and follow-ups are recommended.
Conclusion
The present exercise program can increase the strength of ER and ER:IR ratio and improve SD in overhead athletes.
Acknowledgments: Nothing is mentioned by the authors.
Authors’ Contribution: Naderifar H (First Author), Introduction Writer/Methodologist/Main or Assistant Researcher/Discussion Writer/Statistical Analyst (34%); Ghanbari L (Second Author), Introduction Writer/Methodologist/Main or Assistant Researcher/Discussion Writer/Statistical Analyst (33%); Najafi-Vosough R (Third Author), Introduction Writer/Methodologist/Main or Assistant Researcher/Discussion Writer/Statistical Analyst (33%)
Funding/Support: This article is extracted from research project 140105113374 of Hamadan University of Medical Sciences.









